Page 1816 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1816
1618 Part X Transplantation
a b c d
0201 A A 3101 0201 A A 0101
Antigen 1513 B B 1502 0702 B B 5701
∗
{
HLA-A 0201 0102 Cw Cw 0305 0701 Cw Cw 0602
{
Locus Allele 0701 DRB1 DRB1 0404 0401 DRB1 DRB1 0101
0303 DQB1 DQB1 0302 0304 DQB1 DQB1 0501
A
Mother Father
a c a c a c a c b d
A A A A A A A A A A
B B B B B B B B B B
Cw Cw Cw Cw Cw Cw Cw Cw Cw Cw
DRB1 DRB1 DRB1 DRB1 DRB1 DRB1 DRB1 DRB1 DRB1 DRB1
DQB1 DQB1 DQB1 DQB1 DQB1 DQB1 DQB1 DQB1 DQB1 DQB1
B Patient 1 2 Siblings 3 4
A1 A2 B1 B2 Cw1 Cw2 DRB1-1 DRB1-2 DQB1-1 DQB1-2
Patient 0201 0201 1513 0702 0102 0701 0701 0401 0303 0304
Sibling 2 0201 0101 1513 5701 0102 0602 0701 0101 0303 0601
Patient 0201 0201 0702 1513 0701 0102 0401 0701 0304 0303
C Sibling 3 0201 3101 0702 1502 0701 0305 0401 0404 0304 0302
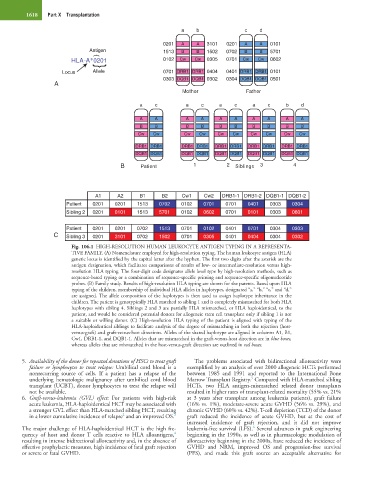
Fig. 106.1 HIGH-RESOLUTION HUMAN LEUKOCYTE ANTIGEN TYPING IN A REPRESENTA-
TIVE FAMILY. (A) Nomenclature employed for high-resolution typing. The human leukocyte antigen (HLA)
genetic locus is identified by the capital letter after the hyphen. The first two digits after the asterisk are the
antigen designation, which facilitates comparisons of results of low- or intermediate-resolution versus high-
resolution HLA typing. The four-digit code designates allele level type by high-resolution methods, such as
sequence-based typing or a combination of sequence-specific priming and sequence-specific oligonucleotide
probes. (B) Family study. Results of high-resolution HLA typing are shown for the parents. Based upon HLA
typing of the children, membership of individual HLA alleles in haplotypes, designated “a,” “b,” “c,” and “d,”
are assigned. The allele composition of the haplotypes is then used to assign haplotype inheritance in the
children. The patient is genotypically HLA matched to sibling 1 and is completely mismatched for both HLA
haplotypes with sibling 4. Siblings 2 and 3 are partially HLA mismatched, or HLA haploidentical, to the
patient, and would be considered potential donors for allogeneic stem cell transplant only if sibling 1 is not
a suitable or willing donor. (C) High-resolution HLA typing of the patient is aligned with typing of the
HLA-haploidentical siblings to facilitate analysis of the degree of mismatching in both the rejection (host-
versus-graft) and graft-versus-host directions. Alleles of the shared haplotype are aligned in columns A1, B1,
Cw1, DRB1-1, and DQB1-1. Alleles that are mismatched in the graft-versus-host direction are in blue boxes,
whereas alleles that are mismatched in the host-versus-graft direction are outlined in red boxes.
5. Availability of the donor for repeated donations of HSCs to treat graft The problems associated with bidirectional alloreactivity were
failure or lymphocytes to treat relapse: Umbilical cord blood is a exemplified by an analysis of over 2000 allogeneic HCTs performed
nonrecurring source of cells. If a patient has a relapse of the between 1985 and 1991 and reported to the International Bone
5
underlying hematologic malignancy after umbilical cord blood Marrow Transplant Registry. Compared with HLA-matched sibling
transplant (UCBT), donor lymphocytes to treat the relapse will HCTs, two HLA antigen-mismatched related donor transplants
not be available. resulted in higher rates of transplant-related mortality (55% vs. 21%
6. Graft-versus-leukemia (GVL) effect: For patients with high-risk at 3 years after transplant among leukemia patients), graft failure
acute leukemia, HLA-haploidentical HCT may be associated with (16% vs. 1%), moderate-severe acute GVHD (56% vs. 29%), and
a stronger GVL effect than HLA-matched sibling HCT, resulting chronic GVHD (60% vs. 42%). T-cell depletion (TCD) of the donor
2
in a lower cumulative incidence of relapse and an improved OS. 3 graft reduced the incidence of acute GVHD, but at the cost of
increased incidence of graft rejection, and it did not improve
6
The major challenge of HLA-haploidentical HCT is the high fre- leukemia-free survival (LFS). Several advances in graft engineering
4
quency of host and donor T cells reactive to HLA alloantigens, beginning in the 1990s, as well as in pharmacologic modulation of
resulting in intense bidirectional alloreactivity and, in the absence of alloreactivity beginning in the 2000s, have reduced the incidence of
effective prophylactic measures, high incidence of fatal graft rejection GVHD and NRM, improved OS and progression-free survival
or severe or fatal GVHD. (PFS), and made this graft source an acceptable alternative for