Page 2172 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2172
Chapter 129 Laboratory Evaluation of Hemostatic and Thrombotic Disorders 1925
Surface Tissue TCT, as indicated by values outside the 95% confidence interval for
activation factor the time to clot of a population of 20 or more normal donors, sug-
gests reduced fibrinogen levels (usually <100 mg/dL), abnormal
fibrinogen function, or the presence of an inhibitor of the exogenous
Intrinsic Extrinsic thrombin (e.g., heparin or a direct thrombin inhibitor). The TCT
can also be elevated if there is interference with fibrin polymerization,
XII, PK which can be caused by elevated levels of fibrinogen degradation
HK products or the presence of a paraprotein. Some drugs, such as val-
XI VII proic acid, also cause elevation of the TCT. 9
IX
VIII EVALUATION OF SPECIFIC COAGULATION
PROTEIN DEFECTS
Common
When the APTT, PT, or TCT indicate a coagulation protein defect,
X the plasma concentration of the coagulation factors should be evalu-
Activated partial V Prothrombin ated. Factor assays determine the nature and severity of coagulation
thromboplastin II time protein defects, and can also be used to monitor factor replacement
time therapy. Coagulation protein defects can take three forms: a true
Fibrinogen protein deficiency; an abnormal protein that cannot participate in its
physiologic function(s); or an inhibitor that targets the active site of
the protein or enhances its clearance. Inherited protein deficiencies
and abnormalities can be caused by deletions, insertions, and
Thrombin missense/nonsense mutations in individual genes. Inhibitors are
time generally immunoglobulins, although abnormally produced endog-
enous heparin, fibronectin, or cryoglobulins can also serve as acquired
inhibitors to coagulation proteins.
If a coagulation protein defect is suspected, clinical laboratory
Fibrin testing can be done with immunologic, chromogenic or clot-based
assays. Clot-based assays for coagulation proteins are functional: they
will be abnormal with both true deficiencies and dysfunctional pro-
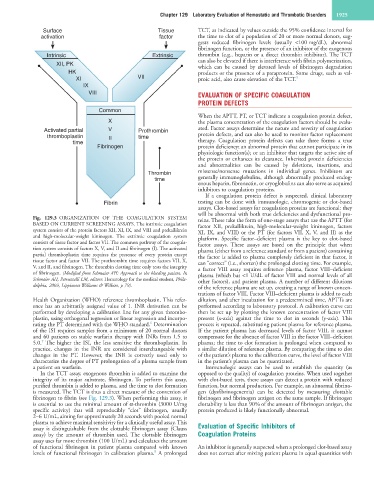
Fig. 129.3 ORGANIZATION OF THE COAGULATION SYSTEM teins. These take the form of one-stage assays that use the APTT (for
BASED ON CURRENT SCREENING ASSAYS. The intrinsic coagulation factor XII, prekallikrein, high-molecular-weight kininogen, factors
system consists of the protein factors XII, XI, IX, and VIII and prekallikrein XI, IX, and VIII) or the PT (for factors VII, X, V, and II) as the
and high-molecular-weight kininogen. The extrinsic coagulation system platform. Specific factor–deficient plasma is the key to clot-based
consists of tissue factor and factor VII. The common pathway of the coagula- factor assays. These assays are based on the principle that when
tion system consists of factors X, V, and II and fibrinogen (I). The activated plasma (either from a reference standard or from a patient) containing
partial thromboplastin time requires the presence of every protein except the factor is added to plasma completely deficient in that factor, it
tissue factor and factor VII. The prothrombin time requires factors VII, X, can “correct” (i.e., shorten) the prolonged clotting time. For example,
V, and II, and fibrinogen. The thrombin clotting time only tests the integrity a factor VIII assay requires reference plasma, factor VIII–deficient
of fibrinogen. (Modified from Schmaier AH: Approach to the bleeding patient. In plasma (which has <1 U/dL of factor VIII and normal levels of all
Schmaier AH, Petruzzelli LM, editors: Hematology for the medical student, Phila- other factors), and patient plasma. A number of different dilutions
delphia, 2003, Lippincott Williams & Wilkins, p 79). of the reference plasma are set up, creating a range of known concen-
trations of factor VIII. Factor VIII–deficient plasma is added to each
Health Organization (WHO) reference thromboplastin. This refer- dilution, and after incubation for a predetermined time, APTTs are
ence has an arbitrarily assigned value of 1. INR derivation can be performed according to laboratory protocol. A calibration curve can
performed by developing a calibration line for any given thrombo- then be set up by plotting the known concentration of factor VIII
plastin, using orthogonal regression or linear regression and incorpo- present (x-axis) against the time to clot in seconds (y-axis). This
6
rating the PT determined with the WHO standard. Determination process is repeated, substituting patient plasma for reference plasma.
of the ISI requires samples from a minimum of 20 normal donors If the patient plasma has decreased levels of factor VIII, it cannot
and 60 patients on stable warfarin therapy with INRs from 1.5 to compensate for the absence of factor VIII in the factor VIII–deficient
7
5.0. The higher the ISI, the less sensitive the thromboplastin. In plasma; the time to clot formation is prolonged when compared to
practice, changes in the INR are considered interchangeable with a similar dilution of reference plasma. By comparing the time to clot
changes in the PT. However, the INR is correctly used only to of the patient’s plasma to the calibration curve, the level of factor VIII
characterize the degree of PT prolongation of a plasma sample from in the patient’s plasma can be quantitated.
a patient on warfarin. Immunologic assays can be used to establish the quantity (as
In the TCT assay, exogenous thrombin is added to examine the opposed to the quality) of coagulation proteins. When used together
integrity of its major substrate, fibrinogen. To perform this assay, with clot-based tests, these assays can detect a protein with reduced
purified thrombin is added to plasma, and the time to clot formation function, but normal production. For example, an abnormal fibrino-
is measured. The TCT is thus a direct measure of the conversion of gen (dysfibrinogenemia) can be detected by measuring clottable
fibrinogen to fibrin (see Fig. 129.3). When performing this assay, it fibrinogen and fibrinogen antigen on the same sample. If fibrinogen
is essential to use the minimal amount of α-thrombin (3000 U/mg clottability is less than 90% of the amount of fibrinogen antigen, the
specific activity) that will reproducibly “clot” fibrinogen, usually protein produced is likely functionally abnormal.
2–6 U/mL, aiming for approximately 20 seconds with pooled normal
plasma to achieve maximal sensitivity for a clinically useful assay. This
assay is distinguishable from the clottable fibrinogen assay (Clauss Evaluation of Specific Inhibitors of
assay) by the amount of thrombin used. The clottable fibrinogen Coagulation Proteins
assay uses far more thrombin (100 U/mL) and calculates the amount
of functional fibrinogen in patient plasma compared with known An inhibitor is generally suspected when a prolonged clot-based assay
8
levels of functional fibrinogen in calibration plasma. A prolonged does not correct after mixing patient plasma in equal quantities with