Page 2335 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2335
Chapter 140 Hypercoagulable States 2077
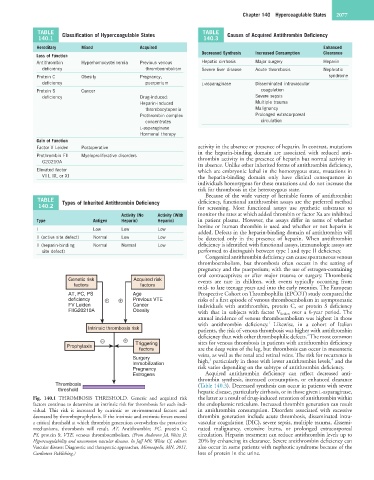
TABLE Classification of Hypercoagulable States TABLE Causes of Acquired Antithrombin Deficiency
140.1 140.3
Hereditary Mixed Acquired Enhanced
Decreased Synthesis Increased Consumption Clearance
Loss of Function
Antithrombin Hyperhomocysteinemia Previous venous Hepatic cirrhosis Major surgery Heparin
deficiency thromboembolism Severe liver disease Acute thrombosis Nephrotic
Protein C Obesity Pregnancy, syndrome
deficiency puerperium L-asparaginase Disseminated intravascular
Protein S Cancer coagulation
deficiency Drug-induced: Severe sepsis
Heparin-induced Multiple trauma
thrombocytopenia Malignancy
Prothrombin complex Prolonged extracorporeal
concentrates circulation
L-asparaginase
Hormonal therapy
Gain of Function
Factor V Leiden Postoperative activity in the absence or presence of heparin. In contrast, mutations
in the heparin-binding domain are associated with reduced anti-
Prothrombin FII Myeloproliferative disorders thrombin activity in the presence of heparin but normal activity in
G20210A
its absence. Unlike other inherited forms of antithrombin deficiency,
Elevated factor which are embryonic lethal in the homozygous state, mutations in
VIII, IX, or XI the heparin-binding domain only have clinical consequences in
individuals homozygous for these mutations and do not increase the
risk for thrombosis in the heterozygous state.
Because of the wide variety of heritable forms of antithrombin
TABLE Types of Inherited Antithrombin Deficiency deficiency, functional antithrombin assays are the preferred method
140.2 for screening. Most functional assays use synthetic substrates to
Activity (No Activity (With monitor the rates at which added thrombin or factor Xa are inhibited
Type Antigen Heparin) Heparin) in patient plasma. However, the assays differ in terms of whether
bovine or human thrombin is used and whether or not heparin is
I Low Low Low
added. Defects in the heparin-binding domain of antithrombin will
II (active site defect) Normal Low Low be detected only in the presence of heparin. When antithrombin
II (heparin-binding Normal Normal Low deficiency is identified with functional assays, immunologic assays are
site defect) performed to distinguish between type I and type II deficiency.
Congenital antithrombin deficiency can cause spontaneous venous
thromboembolism, but thrombosis often occurs in the setting of
pregnancy and the puerperium; with the use of estrogen-containing
oral contraceptives; or after major trauma or surgery. Thrombotic
Genetic risk Acquired risk events are rare in children, with events typically occurring from
factors factors
mid- to late teenage years and into the early twenties. The European
AT, PC, PS Age Prospective Cohort on Thrombophilia (EPCOT) study compared the
deficiency + + Previous VTE risks of a first episode of venous thromboembolism in asymptomatic
FV Leiden Cancer individuals with antithrombin, protein C, or protein S deficiency
FIIG20210A Obesity with that in subjects with factor V Leiden over a 6-year period. The
annual incidence of venous thromboembolism was highest in those
1
with antithrombin deficiency. Likewise, in a cohort of Italian
Intrinsic thrombosis risk patients, the risk of venous thrombosis was higher with antithrombin
2
deficiency than with other thrombophilic defects. The most common
– + Triggering sites for venous thrombosis in patients with antithrombin deficiency
Prophylaxis
factors are the deep veins of the leg, but thrombosis can occur in mesenteric
veins, as well as the renal and retinal veins. The risk for recurrence is
Surgery 3 4
Immobilization high, particularly in those with lower antithrombin levels, and the
Pregnancy risk varies depending on the subtype of antithrombin deficiency.
Estrogens Acquired antithrombin deficiency can reflect decreased anti-
thrombin synthesis, increased consumption, or enhanced clearance
Thrombosis (Table 140.3). Decreased synthesis can occur in patients with severe
threshold hepatic disease, particularly cirrhosis, or in those given L-asparaginase,
Fig. 140.1 THROMBOSIS THRESHOLD. Genetic and acquired risk the latter as a result of drug-induced retention of antithrombin within
factors continue to determine an intrinsic risk for thrombosis for each indi- the endoplasmic reticulum. Increased thrombin generation can result
vidual. This risk is increased by extrinsic or environmental factors and in antithrombin consumption. Disorders associated with excessive
decreased by thromboprophylaxis. If the intrinsic and extrinsic forces exceed thrombin generation include acute thrombosis, disseminated intra-
a critical threshold at which thrombin generation overwhelms the protective vascular coagulation (DIC), severe sepsis, multiple trauma, dissemi-
mechanisms, thrombosis will result. AT, Antithrombin; PC, protein C; nated malignancy, extensive burns, or prolonged extracorporeal
PS, protein S; VTE, venous thromboembolism. (From Anderson JA, Weitz JI: circulation. Heparin treatment can reduce antithrombin levels up to
Hypercoagulability and uncommon vascular diseases. In Jaff MR, White CJ, editors: 20% by enhancing its clearance. Severe antithrombin deficiency can
Vascular disease: Diagnostic and therapeutic approaches, Minneapolis, MN, 2011, also occur in some patients with nephrotic syndrome because of the
Cardiotext Publishing.) loss of protein in the urine.