Page 687 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 687
Chapter 41 Pathobiology of Sickle Cell Disease 579
6
β glu→val
αβ dimer assembly Hb polymerization Hb instability
Hb oxidation
% HbS
Sickling
+ Mechano-
sensitivity Membrane • O 2 −
MCH C HC, heme, Fe H 2 O 2
S
• OH
LOOH
+
K & H O PS
2
loss out
? Vesicles
−S−S− MDA HC/B3
Dehydration C5b-9 clustering
Fragility
+ Ig + Ig
↓ deformability
Trapping Fragmentation Osmotic lysis Erythrophagocytosis
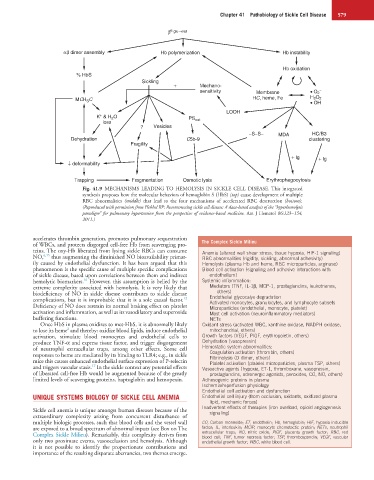
Fig. 41.9 MECHANISMS LEADING TO HEMOLYSIS IN SICKLE CELL DISEASE. This integrated
synthesis proposes how the molecular behaviors of hemoglobin S (HbS) (top) cause development of multiple
RBC abnormalities (middle) that lead to the four mechanisms of accelerated RBC destruction (bottom).
(Reproduced with permission from Hebbel RP: Reconstructing sickle cell disease: A data-based analysis of the “hyperhemolysis
paradigm” for pulmonary hypertension from the perspective of evidence-based medicine. Am J Hematol 86:123−154,
2011.)
accelerates thrombin generation, promotes pulmonary sequestration The Complex Sickle Milieu
of WBCs, and protects disgorged cell-free Hb from scavenging pro-
teins. The oxy-Hb liberated from lysing sickle RBCs can consume Anemia (altered wall shear stress, tissue hypoxia, HIF-1 signaling)
NO, 6,15 thus augmenting the diminished NO bioavailability primar- RBC abnormalities (rigidity, sickling, abnormal adhesivity)
ily caused by endothelial dysfunction. It has been argued that this Hemolysis (plasma Hb and heme, RBC microparticles, arginase)
phenomenon is the specific cause of multiple specific complications Blood cell activation (signaling and adhesive interactions with
of sickle disease, based upon correlations between them and indirect endothelium)
16
hemolytic biomarkers. However, this assumption is belied by the Systemic inflammation:
extreme complexity associated with hemolysis. It is very likely that Mediators (TNF, IL-1β, MCP-1, prostaglandins, leukotrienes,
biodeficiency of NO in sickle disease contributes to sickle disease others)
12
complications, but it is improbable that it is a sole causal factor. Endothelial glycocalyx degradation
Activated monocytes, granulocytes, and lymphocyte subsets
Deficiency of NO does restrain its normal braking effect on platelet Microparticles (endothelial, monocyte, platelet)
activation and inflammation, as well as its vasodilatory and superoxide Mast cell activation (neuroinflammatory mediators)
buffering functions. NETs
Once HbS in plasma oxidizes to met-HbS, it is abnormally likely Oxidant stress (activated WBC, xanthine oxidase, NADPH oxidase,
2
to lose its heme and thereby: oxidize blood lipids, induce endothelial mitochondrial, others)
activation, stimulate blood monocytes and endothelial cells to Growth factors (VEGF, PlGF, erythropoietin, others)
produce TNF-α and express tissue factor, and trigger disgorgement Dehydration (vasopressin)
of neutrophil extracellular traps, among other effects. Some cell Hemostatic system abnormalities:
responses to heme are mediated by its binding to TLR4; e.g., in sickle Coagulation activation (thrombin, others)
Fibrinolysis (D dimer, others)
mice this causes enhanced endothelial surface expression of P-selectin Platelet activation (platelet microparticles, plasma TSP, others)
17
and triggers vascular stasis. In the sickle context any potential effects Vasoactive agents (hypoxia, ET-1, thromboxane, vasopressin,
of liberated cell-free Hb would be augmented because of the greatly prostaglandins, adrenergic agonists, peroxides, CO, NO, others)
limited levels of scavenging proteins, haptoglobin and hemopexin. Adhesogenic proteins in plasma
Ischemia/reperfusion physiology
Endothelial cell activation and dysfunction
UNIQUE SYSTEMS BIOLOGY OF SICKLE CELL ANEMIA Endothelial cell injury (from occlusion, oxidants, oxidized plasma
lipid, mechanic forces)
Inadvertent effects of therapies (iron overload, opioid angiogenesis
Sickle cell anemia is unique amongst human diseases because of the signaling)
extraordinary complexity arising from concurrent disturbance of
multiple biologic processes, such that blood cells and the vessel wall CO, Carbon monoxide; ET, endothelin; Hb, hemoglobin; HIF, hypoxia inducible
are exposed to a broad spectrum of abnormal inputs (see Box on The factor; IL, interleukin; MCIP, monocyte chemotactic protein; NETs, neutrophil
Complex Sickle Milieu). Remarkably, this complexity derives from extracellular traps; NO, nitric oxide; PlGF, placenta growth factor; RBC, red
blood cell; TNF, tumor necrosis factor; TSP, thrombospondin; VEGF, vascular
only two proximate events, vasoocclusion and hemolysis. Although endothelial growth factor; WBC, white blood cell.
it is not possible to identify the proportionate contributions and
importance of the resulting disparate aberrancies, two themes emerge.