Page 2295 - Williams Hematology ( PDFDrive )
P. 2295
2270 Part XII: Hemostasis and Thrombosis Chapter 133: Venous Thrombosis 2271
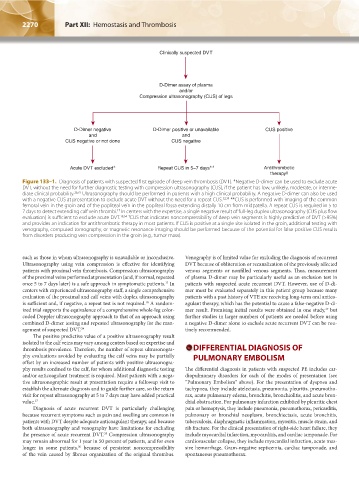
Clinically suspected DVT
D-Dimer assay of plasma
and/or
Compression ultrasonography (CUS) of legs
D-Dimer negative D-Dimer positive or unavailable CUS positive
and and
CUS negative or not done CUS negative
Acute DVT excluded ∗ Repeat CUS in 5–7 days ∗∗ Antithrombotic
therapy ‡
Figure 133–1. Diagnosis of patients with suspected first episode of deep vein thrombosis (DVT). *Negative D-dimer can be used to exclude acute
DVT, without the need for further diagnostic testing with compression ultrasonography (CUS), if the patient has low, unlikely, moderate, or interme-
diate clinical probability. 26,31 Ultrasonography should be performed in patients with a high clinical probability. A negative D-dimer can also be used
with a negative CUS at presentation to exclude acute DVT without the need for a repeat CUS. 32,34 **CUS is performed with imaging of the common
femoral vein in the groin and of the popliteal vein in the popliteal fossa extending distally 10 cm from midpatella. A repeat CUS is required in 5 to
7 days to detect extending calf vein thrombi. In centers with the expertise, a single negative result of full-leg duplex ultrasonography (CUS plus flow
17
evaluation) is sufficient to exclude acute DVT. 18,34 ‡
CUS that indicates noncompressibility of deep vein segments is highly predictive of DVT (>95%)
and provides an indication for antithrombotic therapy in most patients. If CUS is positive at a single site isolated in the groin, additional testing with
venography, computed tomography, or magnetic resonance imaging should be performed because of the potential for false-positive CUS results
from disorders producing vein compression in the groin (e.g., tumor mass).
such as those in whom ultrasonography is unavailable or inconclusive. Venography is of limited value for excluding the diagnosis of recurrent
Ultrasonography using vein compression is effective for identifying DVT because of obliteration or recanalization of the previously affected
patients with proximal vein thrombosis. Compression ultrasonography venous segments or nonfilled venous segments. Thus, measurement
of the proximal veins performed at presentation (and, if normal, repeated of plasma D-dimer may be particularly useful as an exclusion test in
once 5 to 7 days later) is a safe approach in symptomatic patients. In patients with suspected acute recurrent DVT. However, use of D-di-
17
centers with experienced ultrasonography staff, a single comprehensive mer must be evaluated separately in this patient group because many
evaluation of the proximal and calf veins with duplex ultrasonography patients with a past history of VTE are receiving long-term oral antico-
is sufficient and, if negative, a repeat test is not required. A random- agulant therapy, which has the potential to cause a false-negative D-di-
18
ized trial supports the equivalence of a comprehensive whole-leg color- mer result. Promising initial results were obtained in one study, but
37
coded Doppler ultrasonography approach to that of an approach using further studies in larger numbers of patients are needed before using
combined D-dimer testing and repeated ultrasonography for the man- a negative D-dimer alone to exclude acute recurrent DVT can be rou-
agement of suspected DVT. 34 tinely recommended.
The positive predictive value of a positive ultrasonography result
isolated to the calf veins may vary among centers based on expertise and
thrombosis prevalence. Therefore, the number of repeat ultrasonogra- DIFFERENTIAL DIAGNOSIS OF
phy evaluations avoided by evaluating the calf veins may be partially PULMONARY EMBOLISM
offset by an increased number of patients with positive ultrasonogra-
phy results confined to the calf, for whom additional diagnostic testing The differential diagnosis in patients with suspected PE includes car-
and/or anticoagulant treatment is required. Most patients with a nega- diopulmonary disorders for each of the modes of presentation (see
tive ultrasonographic result at presentation require a followup visit to “Pulmonary Embolism” above). For the presentation of dyspnea and
establish the alternate diagnosis and to guide further care, so the return tachypnea, they include atelectasis, pneumonia, pleuritis, pneumotho-
visit for repeat ultrasonography at 5 to 7 days may have added practical rax, acute pulmonary edema, bronchitis, bronchiolitis, and acute bron-
value. 17 chial obstruction. For pulmonary infarction exhibited by pleuritic chest
Diagnosis of acute recurrent DVT is particularly challenging pain or hemoptysis, they include pneumonia, pneumothorax, pericarditis,
because recurrent symptoms such as pain and swelling are common in pulmonary or bronchial neoplasm, bronchiectasis, acute bronchitis,
patients with DVT despite adequate anticoagulant therapy, and because tuberculosis, diaphragmatic inflammation, myositis, muscle strain, and
both ultrasonography and venography have limitations for excluding rib fracture. For the clinical presentation of right-side heart failure, they
the presence of acute recurrent DVT. Compression ultrasonography include myocardial infarction, myocarditis, and cardiac tamponade. For
35
may remain abnormal for 1 year in 50 percent of patients, and for even cardiovascular collapse, they include myocardial infarction, acute mas-
longer in some patients, because of persistent noncompressibility sive hemorrhage, Gram-negative septicemia, cardiac tamponade, and
36
of the vein caused by fibrous organization of the original thrombus. spontaneous pneumothorax.
Kaushansky_chapter 133_p2267-2280.indd 2270 9/18/15 10:52 AM