Page 2314 - Williams Hematology ( PDFDrive )
P. 2314
2288 Part XII: Hemostasis and Thrombosis Chapter 134: Atherothrombosis: Disease Initiation, Progression, and Treatment 2289
Intima at highly susceptible sites of arteries Intima at moderately susceptible sites of arteries
I. Isolated macrophage foam cells
Lipid and cells accumulate
faster and advanced
lesions develop first II. Multiple foam cell layers formed Regression of
at highly susceptible types I–III changes
rather than moderately to normal is possible
susceptible sites
III. Isolated extracellular lipid pools added
IV. Confluent extracellular lipid core formed
Fibrosis of type VI change
adds to type V thickness
V. Fibromuscular tissue layers produced and stiffness
and leads to
loss of lumen
Successive type VI episodes may quickly lead to occlusion
VI. Surface defect, hematoma, thrombosis
VII. Calcification predominates
Regression or change of
lipid in lesion types IV–VI
may result in lesion
VIII. Fibrous tissue changes predominate types VII–VIII
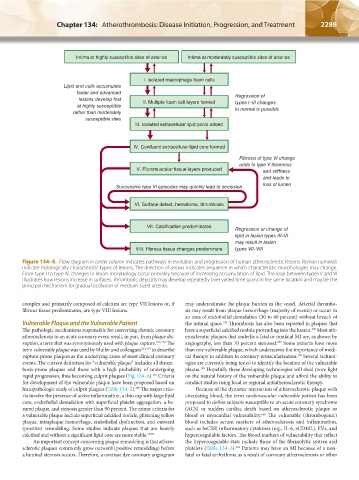
Figure 134–5. Flow diagram in center column indicates pathways in evolution and progression of human atherosclerotic lesions. Roman numerals
indicate histologically characteristic types of lesions. The direction of arrows indicates sequence in which characteristic morphologies may change.
From type I to type IV, changes in lesion morphology occur primarily because of increasing accumulation of lipid. The loop between types V and VI
illustrates how lesions increase in surfaces. Thrombotic deposits may develop repeatedly over varied time spans in the same location and may be the
principal mechanism for gradual occlusion of medium-sized arteries.
complex and primarily composed of calcium are type VII lesions or, if may underestimate the plaque burden in the vessel. Arterial thrombo-
fibrous tissue predominates, are type VIII lesions. sis may result from plaque hemorrhage (majority of events) or occur in
an area of endothelial denudation (30 to 40 percent) without breach of
Vulnerable Plaque and the Vulnerable Patient the intimal space. Thrombosis has also been reported in plaques that
156
The pathologic mechanisms responsible for converting chronic coronary have a superficial calcified nodule protruding into the lumen. Most ath-
156
atherosclerosis to an acute coronary event result, in part, from plaque dis- erosclerotic plaques that underlie a fatal or nonfatal MI are, as shown by
ruption, a term that was synonymously used with plaque rupture. 151,152 The angiography, less than 70 percent stenosed. Some patients have more
157
term vulnerable plaque was used by Muller and colleagues 153,154 to describe than one vulnerable plaque, which underscores the importance of medi-
rupture-prone plaques as the underlying cause of most clinical coronary cal therapy in addition to coronary revascularization. Several technol-
158
events. The current definition for “vulnerable plaque” includes all throm- ogies are currently being tested to identify the location of the vulnerable
bosis-prone plaques and those with a high probability of undergoing plaque. Hopefully these developing technologies will shed more light
159
rapid progression, thus becoming culprit plaques (Fig. 134–6). Criteria on the natural history of the vulnerable plaque and afford the ability to
155
for development of the vulnerable plaque have been proposed based on conduct studies using local or regional antiatherosclerotic therapy.
histopathologic study of culprit plaques (Table 134–2). The major crite- Because of the dynamic interaction of atherosclerotic plaque with
155
ria involve the presence of active inflammation, a thin cap with large lipid circulating blood, the term cardiovascular vulnerable patient has been
core, endothelial denudation with superficial platelet aggregation, a fis- proposed to define subjects susceptible to an acute coronary syndrome
sured plaque, and stenosis greater than 90 percent. The minor criteria for (ACS) or sudden cardiac death based on atherosclerotic plaque or
a vulnerable plaque include superficial calcified nodule, glistening yellow blood or myocardial vulnerability. The vulnerable (thrombogenic)
160
plaque, intraplaque hemorrhage, endothelial dysfunction, and outward blood includes serum markers of atherosclerosis and inflammation,
(positive) remodeling. Some studies indicate plaques that are heavily such as hsCRP, inflammatory cytokines (e.g., IL-6, sCD40L), EVs, and
calcified and without a significant lipid core are more stable. 25,48 hypercoagulable factors. The blood markers of vulnerability that reflect
An important concept concerning plaque remodeling is that athero- the hypercoagulable state include those of the fibrinolytic system and
sclerotic plaques commonly grow outward (positive remodeling) before platelets (Table 134–3). Patients may have an MI because of a non-
161
a luminal stenosis occurs. Therefore, a contrast dye coronary angiogram fatal or fatal arrhythmia as a result of coronary atherosclerosis or other
Kaushansky_chapter 134_p2281-2302.indd 2289 17/09/15 3:49 pm