Page 2356 - Williams Hematology ( PDFDrive )
P. 2356
2330 Part XIII: Transfusion Medicine Chapter 136: Erythrocyte Antigens and Antibodies 2331
GPA/GPB (MNSs), CD235
GPC/GPD (Gerbich), CD236
CD44 (Indian)
CR1 (CD35; Knops) DAF (CD55, Cromer)
CD239 (Lutheran, B-CAM) AChE (Yt)
ICAM-4 (LW), CD242 Dombrock (CD297, ART4)
CD99 (Xg) CD108 (JMH)
CD147 (Ok) CD240 (Rh) Emm
ERMAP (Sc) CD241 (RhAg) CD59
SMIM1 (VEL) Kx
CD238 (Kell) Band 3 (CD233, Diego) NH
ABO 2
Hh (CD173) NH 2 COOH AQP-1 (Colton)
Lewis CD234 (Duffy) Kidd
I ABCB6 (LAN) AQP-3 (GIL)
P1 FORS CD151 (Raph)
P NH 2 ABCG2 (JR)
P k
Outside
COOH NH 2 COOH NH 2 COOH
Type I Type II
Carbohydrate Singlepass Singlepass Multipass GPI-linked
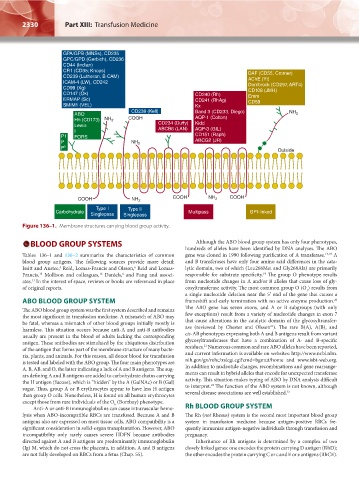
Figure 136–1. Membrane structures carrying blood group activity.
BLOOD GROUP SYSTEMS Although the ABO blood group system has only four phenotypes,
hundreds of alleles have been identified by DNA analyses. The ABO
Tables 136–1 and 136–2 summarize the characteristics of common gene was cloned in 1990 following purification of A transferase. 17,18 A
blood group antigens. The following sources provide more detail: and B transferases have only four amino acid differences in the cata-
Issitt and Anstee, Reid, Lomas-Francis and Olsson, Reid and Lomas- lytic domain, two of which (Leu266Met and Gly268Ala) are primarily
6
5
Francis, Mollison and colleagues, Daniels, and Fung and associ- responsible for substrate specificity. The group O phenotype results
16
19
4
15
ates. In the interest of space, reviews or books are referenced in place from nucleotide changes in A and/or B alleles that cause loss of gly-
11
of original reports. cosyltransferase activity. The most common group O (O ) results from
1
a single nucleotide deletion near the 5′ end of the gene that causes a
ABO BLOOD GROUP SYSTEM frameshift and early termination with no active enzyme production.
20
The ABO blood group system was the first system described and remains The ABO gene has seven exons, and A or B subgroups (with only
the most significant in transfusion medicine. A mismatch of ABO may few exceptions) result from a variety of nucleotide changes in exon 7
be fatal, whereas a mismatch of other blood groups initially mostly is that cause alterations in the catalytic domain of the glycosyltransfer-
21
harmless. This situation occurs because anti-A and anti-B antibodies ase (reviewed by Chester and Olsson ). The rare B(A), A(B), and
usually are present in the blood of adults lacking the corresponding cis-AB phenotypes expressing both A and B antigens result from variant
antigen. These antibodies are stimulated by the ubiquitous distribution glycosyltransferases that have a combination of A- and B-specific
21
of the antigen that forms part of the membrane structure of many bacte- residues. Numerous common and rare ABO alleles have been reported,
ria, plants, and animals. For this reason, all donor blood for transfusion and current information is available on websites: http://www.ncbi.nlm.
is tested and labeled with the ABO group. The four main phenotypes are nih.gov/gv/mhc/xslcgi.cgi?cmd=bgmut/home and www.isbt-web.org.
A, B, AB, and O, the latter indicating a lack of A and B antigens. The sug- In addition to nucleotide changes, recombinations and gene rearrange-
ars defining A and B antigens are added to carbohydrate chains carrying ments can result in hybrid alleles that encode for unexpected transferase
the H antigen (fucose), which is “hidden” by the A (GalNAc) or B (Gal) activity. This situation makes typing of ABO by DNA analysis difficult
22
sugar. Thus, group A or B erythrocytes appear to have less H antigen to interpret. The function of the ABO system is not known, although
than group O cells. Nonetheless, H is found on all human erythrocytes several disease associations are well established. 23
except those from rare individuals of the O (Bombay) phenotype.
h
Anti-A or anti-B immunoglobulins can cause intravascular hemo- Rh BLOOD GROUP SYSTEM
lysis when ABO-incompatible RBCs are transfused. Because A and B The Rh (not Rhesus) system is the second most important blood group
antigens also are expressed on most tissue cells, ABO compatibility is a system in transfusion medicine because antigen-positive RBCs fre-
significant consideration in solid-organ transplantation. However, ABO quently immunize antigen-negative individuals through transfusion and
incompatibility only rarely causes severe HDFN because antibodies pregnancy.
directed against A and B antigens are predominantly immunoglobulin Inheritance of Rh antigens is determined by a complex of two
(Ig) M, which do not cross the placenta, in addition, A and B antigens closely linked genes: one encodes the protein carrying D antigen (RhD);
are not fully developed on RBCs from a fetus (Chap. 55). the other encodes the protein carrying C or c and E or e antigens (RhCE).
Kaushansky_chapter 136_p2327-2352.indd 2330 9/21/15 4:30 PM