Page 671 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 671
644 ParT fivE Allergic Diseases
VERNAL KERATOCONJUNCTIVITIS
VKC is a serious ocular allergy of childhood, comprising 0.1–0.5%
of ocular disease in the developed world but more common and
much more severe in hot, dry countries, especially the Middle
East, West Africa, and the Mediterranean. In the United Kingdom,
VKC is an unusual, self-limiting, often seasonal ocular allergy
that affects children and young adults, especially males (85%)
many of whom have a personal or family history of atopy. The
link with atopy and seasonality is less clearly defined in cooler
climates. Showing
The symptoms are worse in the spring and summer but last corneal plaque
all year in severe disease. Patients complain of marked itching, A
discomfort or pain, photophobia, stringy discharge, blurred
vision, and difficulty opening the eyes in the morning. The ocular
signs may be very asymmetrical. Conjunctival signs are maximal
in the superior tarsal conjunctiva and limbus, and the heavily
inflamed lid may droop (ptosis). The conjunctival surfaces are
hyperemic, edematous, and infiltrated, and a stringy mucoid
discharge is present. The tarsal conjunctiva is densely infiltrated,
with papillae that are often giant (>1 mm in diameter, also known
as cobblestone papillae). The limbus may show discrete swellings Showing corneal
or, less often, diffuse hyperemia and infiltration. The presence vascularization
of small white-chalky deposits (Trantas’ dots) is typical of vernal and mucus thread
limbitis. In the later stages, fine reticular white scarring may be
seen or, in some cases, sclerosing VKC with sclerosis of the upper B
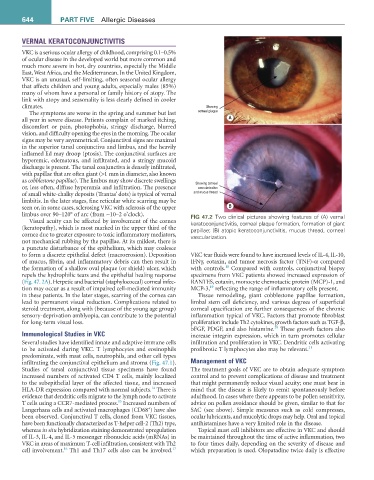
limbus over 90–120° of arc (from ~10–2 o’clock). fiG 47.2 Two clinical pictures showing features of (A) vernal
Visual acuity can be affected by involvement of the cornea keratoconjunctivitis, corneal plaque formation, formation of giant
(keratopathy), which is most marked in the upper third of the papillae; (B) atopic keratoconjunctivitis, mucus thread, corneal
cornea due to greater exposure to toxic inflammatory mediators, vascularization.
not mechanical rubbing by the papillae. At its mildest, there is
a punctate disturbance of the epithelium, which may coalesce
to form a discrete epithelial defect (macroerosion). Deposition VKC tear fluids were found to have increased levels of IL-4, IL-10,
of mucus, fibrin, and inflammatory debris can then result in IFNγ, eotaxin, and tumor necrosis factor (TNF)-α compared
18
the formation of a shallow oval plaque (or shield) ulcer, which with controls. Compared with controls, conjunctival biopsy
repels the hydrophilic tears and the epithelial healing response specimens from VKC patients showed increased expression of
(Fig. 47. 2A). Herpetic and bacterial (staphylococcal) corneal infec- RANTES, eotaxin, monocyte chemotactic protein (MCP)-1, and
19
tion may occur as a result of impaired cell-mediated immunity MCP-3, reflecting the range of inflammatory cells present.
in these patients. In the later stages, scarring of the cornea can Tissue remodeling, giant cobblestone papillae formation,
lead to permanent visual reduction. Complications related to limbal stem cell deficiency, and various degrees of superficial
steroid treatment, along with (because of the young age group) corneal opacification are further consequences of the chronic
sensory-deprivation amblyopia, can contribute to the potential inflammation typical of VKC. Factors that promote fibroblast
for long-term visual loss. proliferation include Th2 cytokines, growth factors such as TGF-β,
20
bFGF, PDGF, and also histamine. These growth factors also
Immunological Studies in VKC increase integrin expression, which in turn promotes cellular
Several studies have identified innate and adaptive immune cells infiltration and proliferation in VKC. Dendritic cells activating
to be activated during VKC. T lymphocytes and eosinophils profibrotic T lymphocytes also may be relevant. 21
predominate, with mast cells, neutrophils, and other cell types
infiltrating the conjunctival epithelium and stroma (Fig. 47.1). Management of VKC
Studies of tarsal conjunctival tissue specimens have found The treatment goals of VKC are to obtain adequate symptom
increased numbers of activated CD4 T cells, mainly localized control and to prevent complications of disease and treatment
to the subepithelial layer of the affected tissue, and increased that might permanently reduce visual acuity; one must bear in
14
HLA-DR expression compared with normal subjects. There is mind that the disease is likely to remit spontaneously before
evidence that dendritic cells migrate to the lymph node to activate adulthood. In cases where there appears to be pollen sensitivity,
15
T cells using a CCR7-mediated process. Increased numbers of advice on pollen avoidance should be given, similar to that for
+
Langerhans cells and activated macrophages (CD68 ) have also SAC (see above). Simple measures such as cold compresses,
been observed. Conjunctival T cells, cloned from VKC tissues, ocular lubricants, and mucolytic drops may help. Oral and topical
have been functionally characterized as T-helper cell-2 (Th2) type, antihistamines have a very limited role in the disease.
whereas in situ hybridization staining demonstrated upregulation Topical mast cell inhibitors are effective in VKC and should
of IL-3, IL-4, and IL-5 messenger ribonucleic acids (mRNAs) in be maintained throughout the time of active inflammation, two
VKC in areas of maximum T-cell infiltration, consistent with Th2 to four times daily, depending on the severity of disease and
16
17
cell involvement. Th1 and Th17 cells also can be involved. which preparation is used. Olopatadine twice daily is effective