Page 969 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 969
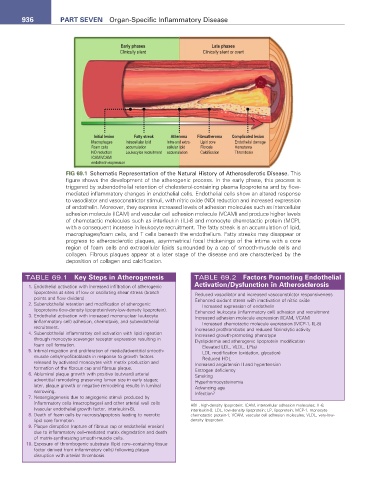
936 Part seven Organ-Specific Inflammatory Disease
Early phases Late phases
Clinically silent Clinically silent or overt
Initial lesion Fatty streak Atheroma Fibroatheroma Complicated lesion
Macrophages Intracellular lipid Intra-and extra- Lipid core Endothelial damage
Foam cells accumulation cellular lipid Fibrosis Hematoma
NO reduction Leukocytes recruitment accumulation Calcification Thrombosis
ICAM/VCAM/
endothelin expression
FIG 69.1 Schematic Representation of the Natural History of Atherosclerotic Disease. This
figure shows the development of the atherogenic process. In the early phase, this process is
triggered by subendothelial retention of cholesterol-containing plasma lipoproteins and by flow-
mediated inflammatory changes in endothelial cells. Endothelial cells show an altered response
to vasodilator and vasoconstrictor stimuli, with nitric oxide (NO) reduction and increased expression
of endothelin. Moreover, they express increased levels of adhesion molecules such as intercellular
adhesion molecule (ICAM) and vascular cell adhesion molecule (VCAM) and produce higher levels
of chemotactic molecules such as interleukin (IL)-8 and monocyte chemotactic protein (MCP),
with a consequent increase in leukocyte recruitment. The fatty streak is an accumulation of lipid,
macrophages/foam cells, and T cells beneath the endothelium. Fatty streaks may disappear or
progress to atherosclerotic plaques, asymmetrical focal thickenings of the intima with a core
region of foam cells and extracellular lipids surrounded by a cap of smooth-muscle cells and
collagen. Fibrous plaques appear at a later stage of the disease and are characterized by the
deposition of collagen and calcification.
TABLE 69.1 Key steps in atherogenesis TABLE 69.2 Factors Promoting endothelial
activation/Dysfunction in atherosclerosis
1. Endothelial activation with increased infiltration of atherogenic
lipoproteins at sites of low or oscillating shear stress (branch Reduced vasodilator and increased vasoconstrictor responsiveness
points and flow dividers). Enhanced oxidant stress with inactivation of nitric oxide
2. Subendothelial retention and modification of atherogenic Increased expression of endothelin
lipoproteins (low-density lipoprotein/very-low-density lipoprotein). Enhanced leukocyte (inflammatory cell) adhesion and recruitment
3. Endothelial activation with increased mononuclear leukocyte Increased adhesion molecule expression (ICAM, VCAM)
(inflammatory cell) adhesion, chemotaxis, and subendothelial Increased chemotactic molecule expression (MCP-1, IL-8)
recruitment. Increased prothrombotic and reduced fibrinolytic activity
4. Subendothelial inflammatory cell activation with lipid ingestion Increased growth-promoting phenotype
through monocyte scavenger receptor expression resulting in Dyslipidemia and atherogenic lipoprotein modification
foam cell formation. Elevated LDL, VLDL, LP(a)
5. Intimal migration and proliferation of medial/adventitial smooth- LDL modification (oxidation, glycation)
muscle cells/myofibroblasts in response to growth factors Reduced HDL
released by activated monocytes with matrix production and Increased angiotensin II and hypertension
formation of the fibrous cap and fibrous plaque. Estrogen deficiency
6. Abluminal plaque growth with positive (outward) arterial Smoking
adventitial remodeling preserving lumen size in early stages; Hyperhomocysteinemia
later, plaque growth or negative remodeling results in luminal Advancing age
narrowing. Infection?
7. Neoangiogenesis due to angiogenic stimuli produced by
inflammatory cells (macrophages) and other arterial wall cells HDL, high-density lipoprotein; ICAM, intercellular adhesion molecules; IL-8,
(vascular endothelial growth factor, interleukin-8). interleukin-8; LDL, low-density lipoprotein; LP, lipoprotein; MCP-1, monocyte
8. Death of foam cells by necrosis/apoptosis leading to necrotic chemotactic protein-1; VCAM, vascular cell adhesion molecules; VLDL, very-low-
lipid core formation. density lipoprotein.
9. Plaque disruption (rupture of fibrous cap or endothelial erosion)
due to inflammatory cell–mediated matrix degradation and death
of matrix-synthesizing smooth-muscle cells.
10. Exposure of thrombogenic substrate (lipid core–containing tissue
factor derived from inflammatory cells) following plaque
disruption with arterial thrombosis.