Page 19 - 2021 Team Member Benefit Guide - English
P. 19
HDHP
Standard Plan Consumer
Plan
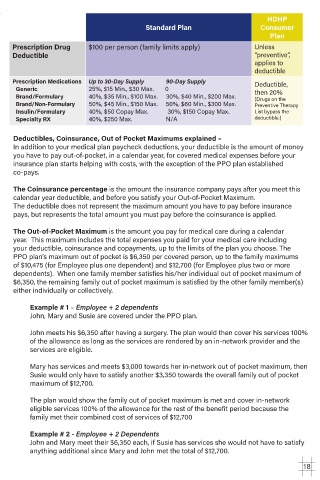
Prescription Drug $100 per person (family limits apply) Unless
Deductible “preventive”,
applies to
deductible
Prescription Medications Up to 30-Day Supply 90-Day Supply Deductible,
Generic 25%, $15 Min., $30 Max. 0 then 20%
Brand/Formulary 40%, $35 Min., $100 Max. 30%, $40 Min., $200 Max. (Drugs on the
Brand/Non-Formulary 50%, $45 Min., $150 Max. 50%, $60 Min., $300 Max. Preventive Therapy
Insulin/Formulary 40%, $50 Copay Max. 30%, $150 Copay Max. List bypass the
Specialty RX 40%, $250 Max. N/A deductible.)
Deductibles, Coinsurance, Out of Pocket Maximums explained –
In addition to your medical plan paycheck deductions, your deductible is the amount of money
you have to pay out-of-pocket, in a calendar year, for covered medical expenses before your
insurance plan starts helping with costs, with the exception of the PPO plan established
co-pays.
The Coinsurance percentage is the amount the insurance company pays after you meet this
calendar year deductible, and before you satisfy your Out-of-Pocket Maximum.
The deductible does not represent the maximum amount you have to pay before insurance
pays, but represents the total amount you must pay before the coinsurance is applied.
The Out-of-Pocket Maximum is the amount you pay for medical care during a calendar
year. This maximum includes the total expenses you paid for your medical care including
your deductible, coinsurance and copayments, up to the limits of the plan you choose. The
PPO plan’s maximum out of pocket is $6,350 per covered person, up to the family maximums
of $10,475 (for Employee plus one dependent) and $12,700 (for Employee plus two or more
dependents). When one family member satisfies his/her individual out of pocket maximum of
$6,350, the remaining family out of pocket maximum is satisfied by the other family member(s)
either individually or collectively.
Example # 1 – Employee + 2 dependents
John, Mary and Susie are covered under the PPO plan.
John meets his $6,350 after having a surgery. The plan would then cover his services 100%
of the allowance as long as the services are rendered by an in-network provider and the
services are eligible.
Mary has services and meets $3,000 towards her in-network out of pocket maximum, then
Susie would only have to satisfy another $3,350 towards the overall family out of pocket
maximum of $12,700.
The plan would show the family out of pocket maximum is met and cover in-network
eligible services 100% of the allowance for the rest of the benefit period because the
family met their combined cost of services of $12,700
Example # 2 - Employee + 2 Dependents
John and Mary meet their $6,350 each, if Susie has services she would not have to satisfy
anything additional since Mary and John met the total of $12,700.
18