Page 5 - 2021 Team Member Benefit Guide - English
P. 5
Mid Year Changes
The only time you can make changes to your benefits outside of your new hire and/or annual
enrollment period is when you experience a family status change event. Team Members must
enroll new dependents or make changes to your benefit elections within 31 days of the family
status change. If you do not make a change within 31 days of the effective date of change your
next opportunity to make changes will be the next annual enrollment period in the Fall of 2021
for coverage starting January 1, 2022.
Submit your family change online in the Dayforce System at https://www.
dayforcehcm.com. To see our Mid-Year Qualifying Events Chart providing
detailed guidance, please click here or scan the QR Code.
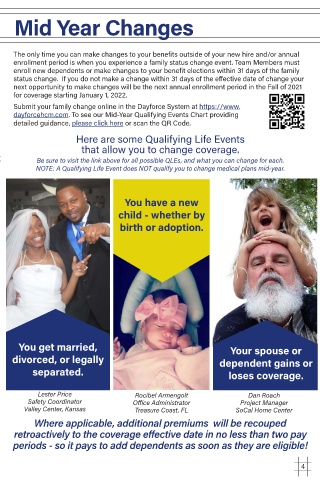
Here are some Qualifying Life Events
that allow you to change coverage.
Be sure to visit the link above for all possible QLEs, and what you can change for each.
NOTE: A Qualifying Life Event does NOT qualify you to change medical plans mid-year.
You have a new
child - whether by
birth or adoption.
You get married, Your spouse or
divorced, or legally dependent gains or
separated. loses coverage.
Lester Price Rocibel Armengolt Dan Roach
Safety Coordinator Office Administrator Project Manager
Valley Center, Kansas Treasure Coast, FL SoCal Home Center
Where applicable, additional premiums will be recouped
retroactively to the coverage effective date in no less than two pay
periods - so it pays to add dependents as soon as they are eligible!
4