Page 253 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 253
CHAPTER 23: Sleep 157
Awake
REM
Stage 1
Stage 2
Stage 3
Young adults
Stage 4
0 1 2 3 4 5 6 7 8
Hours of sleep
Awake
REM
Stage 1
Stage 2
Stage 3
Elderly
Stage 4
0 1 2 3 4 5 6 7 8
Hours of sleep
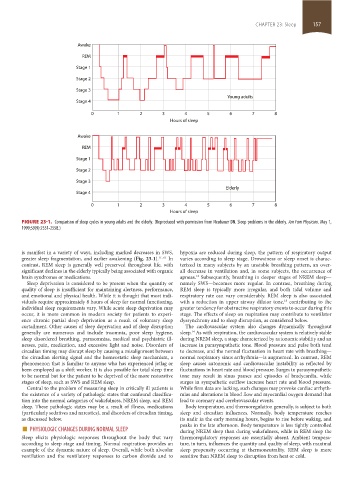
FIGURE 23-1. Comparison of sleep cycles in young adults and the elderly. (Reproduced with permission from Neubauer DN. Sleep problems in the elderly. Am Fam Physician. May 1,
1999;59(9):2551-2558.)
is manifest in a variety of ways, including marked decreases in SWS, hypoxia are reduced during sleep, the pattern of respiratory output
greater sleep fragmentation, and earlier awakening (Fig. 23-1). 11, 61 In varies according to sleep stage. Drowsiness or sleep onset is charac-
contrast, REM sleep is generally well preserved throughout life, with terized in many subjects by an unstable breathing pattern, an over-
significant declines in the elderly typically being associated with organic all decrease in ventilation and, in some subjects, the occurrence of
brain syndromes or medications. apneas. Subsequently, breathing in deeper stages of NREM sleep—
12
Sleep deprivation is considered to be present when the quantity or namely SWS—becomes more regular. In contrast, breathing during
quality of sleep is insufficient for maintaining alertness, performance, REM sleep is typically more irregular, and both tidal volume and
and emotional and physical health. While it is thought that most indi- respiratory rate can vary considerably. REM sleep is also associated
viduals require approximately 8 hours of sleep for normal functioning, with a reduction in upper airway dilator tone, contributing to the
13
individual sleep requirements vary. While acute sleep deprivation may greater tendency for obstructive respiratory events to occur during this
occur, it is more common in modern society for patients to experi- stage. The effects of sleep on respiration may contribute to ventilator
ence chronic partial sleep deprivation as a result of voluntary sleep dyssynchrony and to sleep disruption, as considered below.
curtailment. Other causes of sleep deprivation and of sleep disruption The cardiovascular system also changes dynamically throughout
generally are numerous and include insomnia, poor sleep hygiene, sleep. As with respiration, the cardiovascular system is relatively stable
14
sleep disordered breathing, parasomnias, medical and psychiatric ill- during NREM sleep, a stage characterized by autonomic stability and an
nesses, pain, medication, and excessive light and noise. Disorders of increase in parasympathetic tone. Blood pressure and pulse both tend
circadian timing may disrupt sleep by causing a misalignment between to decrease, and the normal fluctuation in heart rate with breathing—
the circadian alerting signal and the homeostatic sleep mechanism, a normal respiratory sinus arrhythmia—is augmented. In contrast, REM
phenomenon that is familiar to anyone who has experienced jetlag or sleep causes autonomic and cardiovascular instability as reflected by
been employed as a shift worker. It is also possible for total sleep time fluctuations in heart rate and blood pressure. Surges in parasympathetic
to be normal but for the patient to be deprived of the more restorative tone may result in sinus pauses and episodes of bradycardia, while
stages of sleep, such as SWS and REM sleep. surges in sympathetic outflow increase heart rate and blood pressure.
Central to the problem of measuring sleep in critically ill patients is While firm data are lacking, such changes may provoke cardiac arrhyth-
the existence of a variety of pathologic states that confound classifica- mias and alterations in blood flow and myocardial oxygen demand that
tion into the normal categories of wakefulness, NREM sleep, and REM lead to coronary and cerebrovascular events.
sleep. These pathologic states may be a result of illness, medications Body temperature, and thermoregulation generally, is subject to both
(particularly sedatives and narcotics), and disorders of circadian timing, sleep and circadian influences. Normally, body temperature reaches
as discussed below. its nadir in the early morning hours, begins to rise before waking, and
■ PHYSIOLOGIC CHANGES DURING NORMAL SLEEP peaks in the late afternoon. Body temperature is less tightly controlled
during NREM sleep than during wakefulness, while in REM sleep the
Sleep elicits physiologic responses throughout the body that vary thermoregulatory responses are essentially absent. Ambient tempera-
according to sleep stage and timing. Normal respiration provides an ture, in turn, influences the quantity and quality of sleep, with maximal
example of the dynamic nature of sleep. Overall, while both alveolar sleep propensity occurring at thermoneutrality. REM sleep is more
ventilation and the ventilatory responses to carbon dioxide and to sensitive than NREM sleep to disruption from heat or cold.
section02.indd 157 1/13/2015 2:05:07 PM