Page 899 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 899
630 PART 5: Infectious Disorders
severe immunosuppression. 72,73 Asymptomatic primary infection gener-
ally occurs early in life. Rarely, P jirovecii can be found incidentally at
autopsy in the absence of symptoms. It is not clear whether this repre-
sents late infection or early disease not yet manifested clinically.
Pneumocystis remains an important pulmonary pathogen, predomi-
nantly among individuals who were unaware of their HIV status prior to
presentation, or among individuals nonadherent to either prophylactic
strategies or ART in general. Rates of PJP were high in the pre-ART
74
era, with an incidence of 20 cases per 100 person-years in patients
with CD4 cell counts less than 200 cells/mm . The incidence of PJP
3 75
declined markedly after the introduction of ART. Rates of PJP in the
https://kat.cr/user/tahir99/
United States declined 21.5% per year from 1996 to 1998. Similarly,
76
in the EuroSIDA cohort, the incidence of PJP declined from 4.9 cases
per 100 person-years prior to the introduction of ART to 0.3 cases per
100 person-years in 1998. 77
■ CLINICAL AND RADIOLOGIC FEATURES
PJP presents initially as a subacute condition, with a history of progressive
exertional dyspnea accompanied by fever and cough. Occasionally a more
acute illness with progression over the span of a several days may be seen.
Acute dyspnea with chest pain may be indicative of a pneumothorax.
In critically ill patients, the physical examination usually demonstrates
evidence of acute respiratory distress, with surprisingly few adventitious
sounds on auscultation of the chest. Acute hypoxemic respiratory failure
requiring mechanical ventilation has been reported to occur in as many
as 20% of hospitalized patients. Most often this occurs within the first
78
3 days of starting antimicrobial therapy; less frequently acute hypoxemic
respiratory failure develops as a complication of diagnostic bronchoscopy
and rarely as the initial presentation to the emergency room. 78
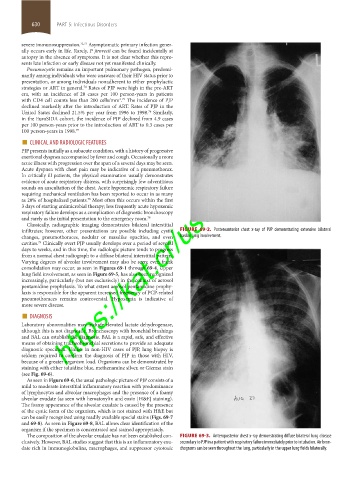
Classically, radiographic imaging demonstrates bilateral interstitial
infiltrates; however, other presentations are possible including cystic FIGURE 69-2. Posteroanterior chest x-ray of PJP demonstrating extensive bilateral
changes, pneumothoraces, nodular or masslike opacities, and even basilar lung involvement.
cavities. Clinically overt PJP usually develops over a period of several
79
days to weeks, and in this time, the radiologic picture tends to progress
from a normal chest radiograph to a diffuse bilateral interstitial pattern.
Varying degrees of alveolar involvement may also be seen; even frank
consolidation may occur, as seen in Figures 69-1 through 69-4. Upper
lung field involvement, as seen in Figure 69-5, has also been recognized
increasingly, particularly (but not exclusively) in the context of aerosol
pentamidine prophylaxis. To what extent aerosol pentamidine prophy-
laxis is responsible for the apparent increased frequency of PCP-related
pneumothoraces remains controversial. Hypoxemia is indicative of
more severe disease.
■ DIAGNOSIS
Laboratory abnormalities may include elevated lactate dehydrogenase,
although this is not diagnostic. Bronchoscopy with bronchial brushings
and BAL can establish the diagnosis. BAL is a rapid, safe, and effective
means of obtaining tracheobronchial secretions to provide an adequate
diagnostic specimen. Unlike in non-HIV cases of PJP, lung biopsy is
seldom required to confirm the diagnosis of PJP in those with HIV,
because of a greater organism load. Organisms can be demonstrated by
staining with either toluidine blue, methenamine silver, or Giemsa stain
(see Fig. 69-6).
As seen in Figure 69-6, the usual pathologic picture of PJP consists of a
mild to moderate interstitial inflammatory reaction with predominance
of lymphocytes and alveolar macrophages and the presence of a foamy
alveolar exudate (as seen with hematoxylin and eosin [H&E] staining).
The foamy appearance of the alveolar exudate is caused by the presence
of the cystic form of the organism, which is not stained with H&E but
can be easily recognized using readily available special stains (Figs. 69-7
and 69-8). As seen in Figure 69-8, BAL allows clear identification of the
organism if the specimen is concentrated and stained appropriately.
The composition of the alveolar exudate has not been established con- FIGURE 69-3. Anteroposterior chest x-ray demonstrating diffuse bilateral lung disease
clusively. However, BAL studies suggest that this is an inflammatory exu- secondary to PJP in a patient with respiratory failure immediately prior to intubation. Air bron-
date rich in immunoglobulins, macrophages, and suppressor cytotoxic chograms can be seen throughout the lung, particularly in the upper lung fields bilaterally.
section05_c61-73.indd 630 1/23/2015 12:48:16 PM