Page 31 - Critical Care Notes
P. 31
4223_Tab01_001-044 29/08/14 10:46 AM Page 25
25
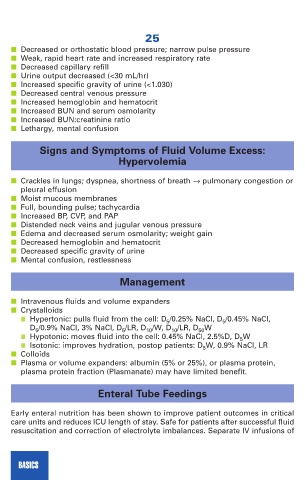
■ Decreased or orthostatic blood pressure; narrow pulse pressure
■ Weak, rapid heart rate and increased respiratory rate
■ Decreased capillary refill
■ Urine output decreased (<30 mL/hr)
■ Increased specific gravity of urine (<1.030)
■ Decreased central venous pressure
■ Increased hemoglobin and hematocrit
■ Increased BUN and serum osmolarity
■ Increased BUN:creatinine ratio
■ Lethargy, mental confusion
Signs and Symptoms of Fluid Volume Excess:
Hypervolemia
■ Crackles in lungs; dyspnea, shortness of breath → pulmonary congestion or
pleural effusion
■ Moist mucous membranes
■ Full, bounding pulse; tachycardia
■ Increased BP, CVP, and PAP
■ Distended neck veins and jugular venous pressure
■ Edema and decreased serum osmolarity; weight gain
■ Decreased hemoglobin and hematocrit
■ Decreased specific gravity of urine
■ Mental confusion, restlessness
Management
■ Intravenous fluids and volume expanders
■ Crystalloids
■ Hypertonic: pulls fluid from the cell: D 5 /0.25% NaCl, D 5 /0.45% NaCl,
D 5 /0.9% NaCl, 3% NaCl, D 5 /LR, D 10 /W, D 10 /LR, D 50 W
■ Hypotonic: moves fluid into the cell: 0.45% NaCl, 2.5%D, D 5 W
■ Isotonic: improves hydration, postop patients: D 5 W, 0.9% NaCl, LR
■ Colloids
■ Plasma or volume expanders: albumin (5% or 25%), or plasma protein,
plasma protein fraction (Plasmanate) may have limited benefit.
Enteral Tube Feedings
Early enteral nutrition has been shown to improve patient outcomes in critical
care units and reduces ICU length of stay. Safe for patients after successful fluid
resuscitation and correction of electrolyte imbalances. Separate IV infusions of
BASICS