Page 533 - Clinical Application of Mechanical Ventilation
P. 533
Critical Care Issues in Mechanical Ventilation 499
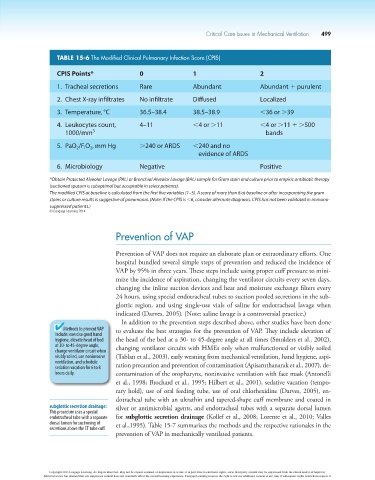
TABLE 15-6 The modified Clinical Pulmonary Infection Score (CPIS)
CPIS Points* 0 1 2
1. Tracheal secretions Rare Abundant Abundant 1 purulent
2. Chest X-ray infiltrates No infiltrate Diffused Localized
3. Temperature, °C 36.5–38.4 38.5–38.9 ,36 or .39
4. Leukocytes count, 4–11 ,4 or .11 ,4 or .11 1 .500
1000/mm 3 bands
5. PaO /F O , mm Hg .240 or ARDS ,240 and no
2
I
2
evidence of ARDS
6. Microbiology Negative Positive
*Obtain Protected Alveolar Lavage (PAL) or Bronchial Alveolar Lavage (BAL) sample for Gram stain and culture prior to empiric antibiotic therapy
(suctioned sputum is suboptimal but acceptable in select patients).
The modified CPIS at baseline is calculated from the first five variables (1–5). A score of more than 6 at baseline or after incorporating the gram
stains or culture results is suggestive of pneumonia. (Note: If the CPIS is ,6, consider alternate diagnosis. CPIS has not been validated in immuno-
suppressed patients.)
© Cengage Learning 2014
Prevention of VAP
Prevention of VAP does not require an elaborate plan or extraordinary efforts. One
hospital bundled several simple steps of prevention and reduced the incidence of
VAP by 95% in three years. These steps include using proper cuff pressure to mini-
mize the incidence of aspiration, changing the ventilator circuits every seven days,
changing the inline suction devices and heat and moisture exchange filters every
24 hours, using special endotracheal tubes to suction pooled secretions in the sub-
glottic region, and using single-use vials of saline for endotracheal lavage when
indicated (Darves, 2005). (Note: saline lavage is a controversial practice.)
In addition to the prevention steps described above, other studies have been done
Methods to prevent VAP to evaluate the best strategies for the prevention of VAP. They include elevation of
include: exercise good hand
hygiene, elevate head of bed the head of the bed at a 30- to 45-degree angle at all times (Smulders et al., 2002),
at 30- to 45-degree angle, changing ventilator circuits with HMEs only when malfunctioned or visibly soiled
change ventilator circuit when
visibly soiled, use noninvasive (Tablan et al., 2003), early weaning from mechanical ventilation, hand hygiene, aspi-
ventilation, and schedule
sedation vacation for 6 to 8 ration precaution and prevention of contamination (Apisarnthanarak et al., 2007), de-
hours daily. contamination of the oropharynx, noninvasive ventilation with face mask (Antonelli
et al., 1998; Brochard et al., 1995; Hilbert et al., 2001), sedative vacation (tempo-
rary hold), use of oral feeding tube, use of oral chlorhexidine (Darves, 2005), en-
dotracheal tube with an ultrathin and tapered-shape cuff membrane and coated in
subglottic secretion drainage: silver or antimicrobial agents, and endotracheal tubes with a separate dorsal lumen
This procedure uses a special
endotracheal tube with a separate for subglottic secretion drainage (Kollef et al., 2008; Lorente et al., 2010; Valles
dorsal lumen for suctioning of et al.,1995). Table 15-7 summarizes the methods and the respective rationales in the
secretions above the ET tube cuff.
prevention of VAP in mechanically ventilated patients.
Copyright 2013 Cengage Learning. All Rights Reserved. May not be copied, scanned, or duplicated, in whole or in part. Due to electronic rights, some third party content may be suppressed from the eBook and/or eChapter(s).
Editorial review has deemed that any suppressed content does not materially affect the overall learning experience. Cengage Learning reserves the right to remove additional content at any time if subsequent rights restrictions require it.