Page 266 - Cardiac Nursing
P. 266
009
1
1
21
6/2
009
21
M
M
Pa
7 A
0:4
0:4
7 A
q
q
44.
q
3
xd
xd
0/0
0/0
6/2
3
44.
1-2
1-2
Pa
ara
ara
10_
t
p
p
t
10_
LWB
LWB
LWBK340-c10_ p p pp211-244.qxd 30/06/2009 10:47 AM Page 242 Aptara
K34
0-c
0-c
K34
A
42
g
g
e 2
g
42
e 2
A
p
242 P A R T III / Assessment of Heart Disease
1 1
2 2
3 3
■ Figure 10-35 Adventitious breath sounds. (A) Crackles. (B)
5 4 4 5
Wheezes. (C) Pleural friction rubs.
6 6
ventilation of basilar tissue), but may progress to all portions of
the lung fields.
Wheezes are continuous, musical sounds from rapid air move-
ment through constricted airways. They are heard most often on
expiration but can be heard during both inspiration and expira- ■ Figure 10-36 Sequence of anterior percussion and auscultation.
tion (Fig. 10-35B). Although wheezes are characteristic of ob-
structive lung disease, they can be caused by interstitial pul-
monary edema compressing small airways. -Adrenergic before initiating a diet. Liver engorgement occurs because of de-
blocking agents, such as propranolol, may precipitate airway creased venous return secondary to right ventricular failure. Urine
narrowing, especially in patients with underlying pulmonary output is an important indicator of cardiac output. In a patient
disease. A fixed wheeze is characteristic of an endobronchial who is unable to void (e.g., secondary to strict bed rest or after at-
mass or tumor. ropine sulfate administration) or who has not voided despite ade-
Transmitted voice sounds may be louder and clearer than nor- quate fluid intake, always assess for bladder distention before ini-
mal (bronchophony, whispered pectoriloquy) when heard tiating other measures.
through the chest wall. The quality of voice sounds may have a
nasal or bleating character (egophony). Transmitted voice sounds Inspection
suggest consolidation of lung tissue. Observe the abdomen for symmetry and visible peristalsis. Note
Pleural friction rubs result from inflamed pleura rubbing to- the presence of abdominal distention. Abdominally localized obe-
gether. A pleural friction rub, characteristic of pleuritis, is a coarse, sity (waist circumference 35 inches for women or 40 inches
grating sound that can be heard on inspiration and expiration for men) is associated with coronary artery disease, adult-onset di-
(Fig. 10-35C). abetes mellitus, and metabolic syndrome.
Anterior Chest Ausculation
Auscultate the abdomen after observation because palpation and
Palpation. Tenderness of the pectoral muscles or costal carti- percussion can either increase or diminish bowel sounds. Gently
lage suggests a musculoskeletal origin of chest pain. Respiratory ex- place the diaphragm of the stethoscope on the abdomen. Listen
cursion is assessed in the same manner as on the posterior chest, ex- over all quadrants. Normal bowel sounds consist of clicks and gur-
cept that the examiner’s thumbs are placed along each costal gles, at a frequency of 5 to 34 per minute. It is necessary to listen
margin. Assess vocal or tactile fremitus. Fremitus normally is di- for 2 minutes or more to determine that bowel sounds are absent.
minished over the precordium.
Borborygmi (prolonged gurgles of hyperperistalsis) also may be
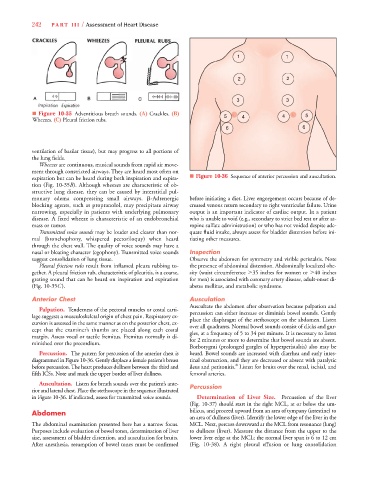
Percussion. The pattern for percussion of the anterior chest is heard. Bowel sounds are increased with diarrhea and early intes-
diagrammed in Figure 10-36. Gently displace a female patient’s breast tinal obstruction, and they are decreased or absent with paralytic
8
before percussion. The heart produces dullness between the third and ileus and peritonitis. Listen for bruits over the renal, ischial, and
fifth ICSs. Note and mark the upper border of liver dullness. femoral arteries.
Auscultation. Listen for breath sounds over the patient’s ante- Percussion
rior and lateral chest. Place the stethoscope in the sequence illustrated
in Figure 10-36. If indicated, assess for transmitted voice sounds. Determination of Liver Size. Percussion of the liver
(Fig. 10-37) should start in the right MCL, at or below the um-
Abdomen bilicus, and proceed upward from an area of tympany (intestine) to
an area of dullness (liver). Identify the lower edge of the liver in the
The abdominal examination presented here has a narrow focus. MCL. Next, percuss downward at the MCL from resonance (lung)
Purposes include evaluation of bowel tones, determination of liver to dullness (liver). Measure the distance from the upper to the
size, assessment of bladder distention, and auscultation for bruits. lower liver edge at the MCL; the normal liver span is 6 to 12 cm
After anesthesia, resumption of bowel tones must be confirmed (Fig. 10-38). A right pleural effusion or lung consolidation