Page 465 - Cardiac Nursing
P. 465
LWBK340-c20_p439-459.qxd 6/29/09 11:29 PM Page 441 Aptara Inc.
C HAP TE R 2 0 / Cardiac Catheterization 441
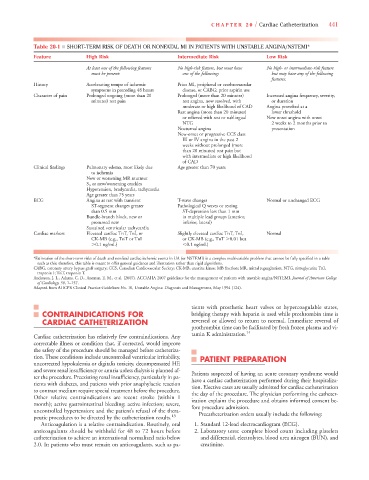
Table 20-1 ■ SHORT-TERM RISK OF DEATH OR NONFATAL MI IN PATIENTS WITH UNSTABLE ANGINA/NSTEMI*
Feature High Risk Intermediate Risk Low Risk
At least one of the following features No high-risk feature, but must have No high- or intermediate-risk feature
must be present: one of the following: but may have any of the following
features:
History Accelerating tempo of ischemic Prior MI, peripheral or cerebrovascular
symptoms in preceding 48 hours disease, or CABG; prior aspirin use
Character of pain Prolonged ongoing (more than 20 Prolonged (more than 20 minutes) Increased angina frequency, severity,
minutes) rest pain rest angina, now resolved, with or duration
moderate or high likelihood of CAD Angina provoked at a
Rest angina (more than 20 minutes) lower threshold
or relieved with rest or sublingual New onset angina with onset
NTG 2 weeks to 2 months prior to
Nocturnal angina presentation
New-onset or progressive CCS class
III or IV angina in the past 2
weeks without prolonged (more
than 20 minutes) rest pain but
with intermediate or high likelihood
of CAD
Clinical findings Pulmonary edema, most likely due Age greater than 70 years
to ischemia
New or worsening MR murmur
S 3 or new/worsening crackles
Hypotension, bradycardia, tachycardia
Age greater than 75 years
ECG Angina at rest with transient T-wave changes Normal or unchanged ECG
ST-segment changes greater Pathological Q waves or resting
than 0.5 mm ST-depression less than 1 mm
Bundle-branch block, new or in multiple lead groups (anterior,
presumed new inferior, lateral)
Sustained ventricular tachycardia
Cardiac markers Elevated cardiac TnT, TnI, or Slightly elevated cardiac TnT, TnI, Normal
CK-MB (e.g., TnT or TnI or CK-MB (e.g., TnT 0.01 but
0.1 ng/mL) 0.1 ng/mL)
*Estimation of the short-term risks of death and nonfatal cardiac ischemic events in UA (or NSTEMI) is a complex multivariable problem that cannot be fully specified in a table
such as this; therefore, this table is meant to offer general guidance and illustration rather than rigid algorithms.
CABG, coronary artery bypass graft surgery; CCS, Canadian Cardiovascular Society; CK-MB, creatine kinase MB fraction; MR, mitral regurgitation; NTG, nitroglycerin; TnI,
troponin I; TnT, troponin T.
Anderson, J. L., Adams, C. D., Antman, E. M., et al. (2007). ACC/AHA 2007 guidelines for the management of patients with unstable angina/NSTEMI. Journal of American College
of Cardiology, 50, 1–157.
Adapted from AHCPR Clinical Practice Guidelines No. 10, Unstable Angina: Diagnosis and Management, May 1994 (124).
tients with prosthetic heart valves or hypercoagulable states,
CONTRAINDICATIONS FOR bridging therapy with heparin is used while prothrombin time is
CARDIAC CATHETERIZATION reversed or allowed to return to normal. Immediate reversal of
prothrombin time can be facilitated by fresh frozen plasma and vi-
tamin K administration. 14
Cardiac catheterization has relatively few contraindications. Any
correctable illness or condition that, if corrected, would improve
the safety of the procedure should be managed before catheteriza-
tion. These conditions include uncontrolled ventricular irritability, PATIENT PREPARATION
uncorrected hypokalemia or digitalis toxicity, decompensated HF,
and severe renal insufficiency or anuria unless dialysis is planned af- Patients suspected of having an acute coronary syndrome would
ter the procedure. Preexisting renal insufficiency, particularly in pa- have a cardiac catheterization performed during their hospitaliza-
tients with diabetes, and patients with prior anaphylactic reaction tion. Elective cases are usually admitted for cardiac catheterization
to contrast medium require special treatment before the procedure. the day of the procedure. The physician performing the catheter-
Other relative contraindications are recent stroke (within 1 ization explains the procedure and obtains informed consent be-
month); active gastrointestinal bleeding; active infection; severe, fore procedure admission.
uncontrolled hypertension; and the patient’s refusal of the thera- Precatheterization orders usually include the following:
peutic procedures to be directed by the catheterization results. 13
Anticoagulation is a relative contraindication. Routinely, oral 1. Standard 12-lead electrocardiogram (ECG).
anticoagulants should be withheld for 48 to 72 hours before 2. Laboratory tests: complete blood count including platelets
catheterization to achieve an international normalized ratio below and differential, electrolytes, blood urea nitrogen (BUN), and
2.0. In patients who must remain on anticoagulants, such as pa- creatinine.