Page 651 - Cardiac Nursing
P. 651
CHAPTER 26 / Mechanical Circulatory Assist Devices 627
refill the balloon and catheter at least every 2 hours. An abrupt Complications
loss of the pressure peak may indicate the development of a bal-
loon or catheter leak. Occasionally, augmentation greater than IABP therapy carries a relatively low risk of additional morbidity
the systolic pressure is not achievable because the balloon is too in a generally sick population. In the series of nearly 17,000 pa-
small relative to the aorta. Ideally, the balloon should occlude tients with IABPs placed (from 1996 to 2000) mentioned above,
85% to 90% of the aorta when fully inflated. If there is a size the incidence of any complication was 7% and major complica-
mismatch, diastolic augmentation pressure may be reduced, tions (i.e., severe bleeding, major acute limb ischemia, death from
7
and may even be less than the patient’s systole. IABP insertion, or failure) was 2.6%. Vascular complications
n Criterion 4. The balloon deflation should occur at the end of di- have been reported to range from 6% to 25% of cases depending
14–16
astole. Proper deflation results in a drop in pressure at the end of on the report. Vascular injuries include plaque dislodgement,
diastole. This drop in pressure creates an end-diastolic pressure dissection, laceration, and compromise of the circulation to the
much lower than diastolic pressure without the balloon effect. distal extremity. Peripheral nerve injury is another possible com-
Timing is adjusted so that the lowest pressure possible is plication of insertion (particularly if a cut down approach is used).
achieved. It is important to make sure that the systolic upstroke Compromised circulation can occur any time during IABP ther-
that follows is straight and that a sharp, V-shaped configuration apy as a result of the presence of the indwelling catheter, com-
is present. The V shape indicates that systole began immediately partment syndrome, or embolus from thrombus formation along
17
after deflation. Any plateau indicates that deflation occurred too the catheter or on the balloon. The incidence of limb ischemia
17,18
early, diminishing (or obliterating) the intended reduction in af- ranges from 5% to 35%. Although intravenous heparin is
terload. Late deflation, on the other hand, results in higher im- generally used with IABP, there is little evidence that heparin re-
pedance because the balloon remains inflated at the onset of sys- duces limb ischemia, and one randomized trial of 153 patients did
19
tolic ejection, creating more work for the LV. An end-diastolic not find a difference in such events.
pressure that is the same or greater than the end-diastolic pres- Complications are more common in patients with peripheral
sure without balloon assistance is evidence of late deflation. The vascular occlusive disease, in women, those who are smaller (body
2
systolic pressure in the following beat may be the same or lower surface area [BSA] ,1.8 m ), and in patients with a history of
7,17,20–23
than the unassisted systole because of the inability of the failing stroke, transient ischemic attacks, and diabetes. Risk is
ventricle to work against the higher impedance to ejection. decreased with sheathless insertion and with smaller balloon
n Criterion 5. Finally, the observer should note what effect bal- sizes. 22,24,25 In addition, operator’s and hospital-staff’s experience
26
loon deflation has on the next systolic pressure, for the reasons likely play a part. Nurses monitor for and prevent compromised
just described. The goal is to ensure that the lower systolic pres- circulation by carefully assessing peripheral perfusion; preventing
sure that follows balloon deflation is caused by afterload reduc- the patient from flexing the hip of the affected extremity, which
tion and not by improper timing, which resulted in late may compromise blood flow; and maintaining coagulation times
deflation. Proper balloon fit has an impact on the ability to within prescribed parameters by careful titration of any prescribed
achieve afterload reduction. If the balloon size is small, then anticoagulants. The nurse should be aware that multiple or pro-
volume displacement may have less of an effect on lowering longed attempts at insertion increase the risk of vascular injury
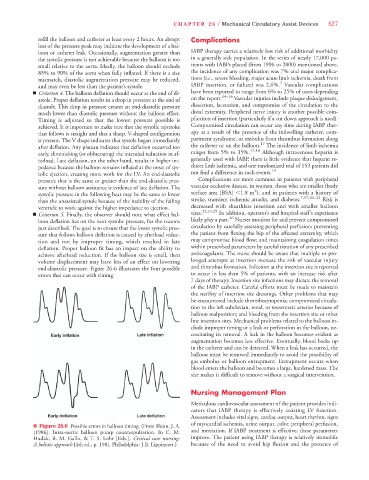
end-diastolic pressure. Figure 26-6 illustrates the four possible and thrombus formation. Infection at the insertion site is reported
errors that can occur with timing. to occur in less than 5% of patients, with an increase risk after
7 days of therapy. Insertion site infections may dictate the removal
of the IABP catheter. Careful efforts must be made to maintain
the sterility of insertion site dressings. Other problems that may
be encountered include thrombocytopenia; compromised circula-
tion to the left subclavian, renal, or mesenteric arteries because of
balloon malposition; and bleeding from the insertion site or other
line insertion sites. Mechanical problems related to the balloon in-
clude improper timing or a leak or perforation in the balloon, ne-
cessitating its removal. A leak in the balloon becomes evident as
augmentation becomes less effective. Eventually, blood backs up
in the catheter and can be detected. When a leak has occurred, the
balloon must be removed immediately to avoid the possibility of
gas embolus or balloon entrapment. Entrapment occurs when
blood enters the balloon and becomes a large, hardened mass. The
size makes it difficult to remove without a surgical intervention.
Nursing Management Plan
Meticulous cardiovascular assessment of the patient provides indi-
cators that IABP therapy is effectively assisting LV function.
Assessment includes vital signs, cardiac output, heart rhythm, signs
of myocardial ischemia, urine output, color, peripheral perfusion,
n Figure 26-6 Possible errors in balloon timing. (From Shinn, J. A.
[1986]. Intra-aortic balloon pump counterpulsation. In C. M. and mentation. If IABP treatment is effective, these parameters
Hudak, B. M. Gallo, & T. S. Lohr [Eds.], Critical care nursing: improve. The patient using IABP therapy is relatively immobile
A holistic approach [4th ed., p. 198]. Philadelphia: J.B. Lippincott.) because of the need to avoid hip flexion and the presence of