Page 652 - Cardiac Nursing
P. 652
628 P AR T IV / Pathophysiology and Management of Heart Disease
multiple invasive monitoring and infusion lines. Often, due to occurring during the patient’s diastole or asynchronous with
their critical condition, patients will be intubated and on ventila- their cardiac cycle. Although it was previously thought that pul-
tor support. Care must be taken to prevent or minimize atelecta- satile flow patterns were more desirable, studies have shown
sis. These patients also are at greater risk for respiratory tract in- equivalent flow generation and clinical outcomes. 27,28 Continu-
fection. Careful suctioning technique and prevention of ous flow pumps are generally smaller, because they do not re-
aspiration reduce this risk. quire a reservoir chamber. The remainder of this section will
Prolonged hypotension from the shock state may jeopardize describe several assistive devices in order of increasing durations
renal function. Monitoring urine output and quality closely may of use.
contribute to early recognition and treatment of renal dysfunc-
tion, thus avoiding acute renal failure. Psychosocial support of Short-Term Ventricular Assist Devices
the patient and family is also important. The patient requires in-
terventions that minimize stress, disorientation, and sleep depri- Percutaneous Axial Flow Pump
vation. Families benefit from honest communication and help Axial flow pumps work on the principle of the Archimedes screw.
with the interpretation of the patient’s condition. Nursing Care They are composed of a single cannula which is placed retrograde
Plan 26-1 outlines a plan of care for the patient on IABP therapy. across the aortic valve into the left ventricle. Although they may
Because this patient is experiencing acute LV failure or cardio- be placed surgically, a femoral artery approach can be used. 29,30
genic shock, many nursing diagnoses used for those conditions The screw turns and draws blood out of the LV and ejects it into
apply. The plan of care that is outlined focuses on issues unique the ascending aorta beyond the aortic valve. Figure 26-7 depicts
to IABP therapy. The Nursing Care Plan, originally written by the device. Currently available devices include the Impella 2.5 and
Laurent and Shinn for the 5th edition of Cardiac Nursing, has 5.0 microaxial flow devices (Abiomed, Inc., Danvers, MA).
been placed at the end of this chapter. Because the position of the outflow area must be confirmed to
be on the aortic side of the aortic valve, either fluoroscopic or
echocardiographic guidance must be utilized. These devices can
generate (nonpulsatile) flows of up to 2.5 or 5.0 L/min (de-
OTHER MECHANICAL pending on the model). Anticoagulation is required. Risks include
CIRCULATORY ASSIST DEVICES hemolysis and thrombocytopenia, which are often transient; sig-
nificant aortic valve disease (stenosis or regurgitation) can con-
An IABP is only able to augment cardiac output marginally (500 traindicate its use. 31
to 800 mL/min). Thus, with profound ventricular failure, IABP
therapy may provide insufficient assistance, and more aggressive
therapy may need to be considered. In recent years, a number of
other mechanical circulatory assist devices have been developed
for short-, intermediate-, and long-term use.
Indications and Contraindications
Indications for mechanical assistance include support/off-loading
of the heart during high-risk PCI, weaning from cardiopulmonary
bypass, as a bridge to recovery (from acute MI or acute myocardi-
tis), as a bridge to transplant, or as a bridge to another device (e.g.,
a more permanent device) or for so-called “destination therapy” in
patients who are not transplant candidates. Device selection
depends on patient factors such as anticipated duration of need,
patient size, as well as local experience and patient preference.
Contraindications to most of these devices include severe aor-
tic or peripheral vascular disease (i.e., dissection, atherosclerosis,
or aneurysm), LV or atrial thrombi, coagulopathy, uncontrolled
sepsis, significant aortic valve stenosis or regurgitation, recent
stroke or neurologic injury, or when invasive or heroic therapy
would clearly be futile or inappropriate.
Mechanism of Support
Most (but not all) circulatory assist devices are designed to replace
the pumping function of the left (or sometimes right or both)
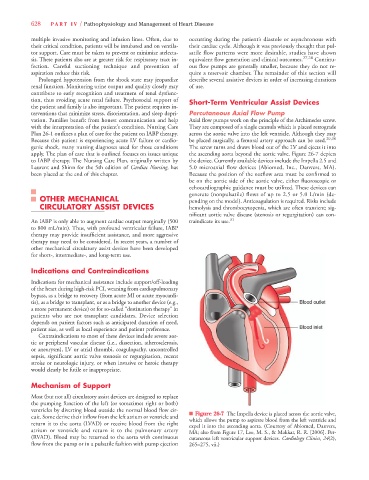
ventricles by diverting blood outside the normal blood flow cir- n Figure 26-7 The Impella device is placed across the aortic valve,
cuit. Some derive their inflow from the left atrium or ventricle and which allows the pump to aspirate blood from the left ventricle and
return it to the aorta (LVAD) or receive blood from the right expel it into the ascending aorta. (Courtesy of Abiomed, Danvers,
atrium or ventricle and return it to the pulmonary artery MA; also from Figure 17, Lee, M. S., & Makkar, R. R. [2006]. Per-
(RVAD). Blood may be returned to the aorta with continuous cutaneous left ventricular support devices. Cardiology Clinics, 24(2),
flow from the pump or in a pulsatile fashion with pump ejection 265–275, vii.)