Page 83 - Cardiac Nursing
P. 83
6/3
0/2
6/3
0
0
1
1
009
0/2
009
68.
q
68.
2-0
2-0
xd
0
xd
q
q
5:3
p
p
9 A
e 5
9 A
r
r
ta
p
ta
Pa
Pa
3
5:3
3
g
e 5
g
Pa
g
04
K34
0-c
02_
LWB K34 0-c 02_ p p pp042-068.qxd 06/30/2009 15:33 Page 59 Aptara a a
LWB
LWBK340-c02_
04
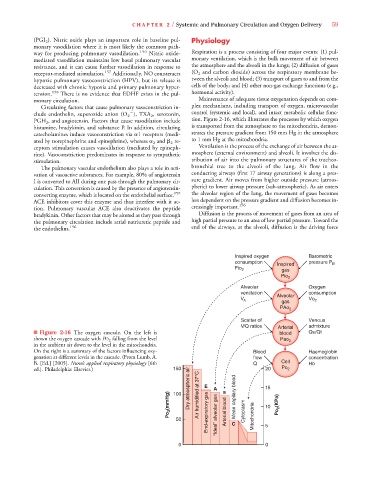
C HAPTER 2 / Systemic and Pulmonary Circulation and Oxygen Delivery 59
(PGI 2 ). Nitric oxide plays an important role in baseline pul- Physiology
monary vasodilation where it is most likely the common path-
way for producing pulmonary vasodilation. 156 Nitric oxide- Respiration is a process consisting of four major events: (1) pul-
mediated vasodilation maintains low basal pulmonary vascular monary ventilation, which is the bulk movement of air between
resistance, and it can cause further vasodilation in response to the atmosphere and the alveoli in the lungs; (2) diffusion of gases
receptor-mediated stimulation. 157 Additionally, NO counteracts (O 2 and carbon dioxide) across the respiratory membrane be-
hypoxic pulmonary vasoconstriction (HPV), but its release is tween the alveoli and blood; (3) transport of gases to and from the
decreased with chronic hypoxia and primary pulmonary hyper- cells of the body; and (4) other non-gas exchange functions (e.g.,
tension. 158 There is no evidence that EDHF exists in the pul- hormonal activity).
monary circulation. Maintenance of adequate tissue oxygenation depends on com-
Circulating factors that cause pulmonary vasoconstriction in- plex mechanisms, including transport of oxygen, microvascular
clude endothelin, superoxide anion (O 2 ), TXA 2 , serotonin, control (systemic and local), and intact metabolic cellular func-
PGH 2 , and angiotensin. Factors that cause vasodilation include tion. Figure 2-16, which illustrates the processes by which oxygen
histamine, bradykinin, and substance P. In addition, circulating is transported from the atmosphere to the mitochondria, demon-
catecholamines induce vasoconstriction via 1 receptors (medi- strates the pressure gradient from 150 mm Hg in the atmosphere
ated by norepinephrine and epinephrine), whereas 2 and 2 re- to 1 mm Hg at the mitochondria.
ceptors stimulation causes vasodilation (mediated by epineph- Ventilation is the process of the exchange of air between the at-
rine). Vasoconstriction predominates in response to sympathetic mosphere (external environment) and alveoli. It involves the dis-
stimulation. tribution of air into the pulmonary structures of the tracheo-
The pulmonary vascular endothelium also plays a role in acti- bronchial tree to the alveoli of the lung. Air flow in the
vation of vasoactive substances. For example, 80% of angiotensin conducting airways (first 17 airway generations) is along a pres-
I is converted to AII during one pass through the pulmonary cir- sure gradient. Air moves from higher outside pressure (atmos-
culation. This conversion is caused by the presence of angiotensin- pheric) to lower airway pressure (sub-atmospheric). As air enters
converting enzyme, which is located on the endothelial surface. 159 the alveolar region of the lung, the movement of gases becomes
ACE inhibitors cover this enzyme and thus interfere with it ac- less dependent on the pressure gradient and diffusion becomes in-
156
tion. Pulmonary vascular ACE also deactivates the peptide creasingly important.
bradykinin. Other factors that may be altered as they pass through Diffusion is the process of movement of gases from an area of
the pulmonary circulation include atrial natriuretic peptide and high partial pressure to an area of low partial pressure. Toward the
the endothelins. 156 end of the airways, at the alveoli, diffusion is the driving force
Inspired oxygen Barometric
consumption pressure P
i i i i i i i i i i i i i
Inspired d d d d d d d d d d d d d d d d d B
Inspired
Inspired
Inspired
Inspired
I I I I I I I I I I I I I Inspired
Fio 2 gas
Pio 2
Alveolar Oxygen
ventilation Alveolar consumption
Al Al Al Al Al Al Al Al Al Al Al Al Al Al Al eolar
Alveolar
Alveolar
Alveolar
Alveolar
Alveolar
Alveolar
Alveolar
Alveolar
Alveolar
l l l l l l l l l l l l l l
Alveolar
Alveolar
Alveolar
Alveolar
Alveolar
V V A gas Vo 2
PAo 2 2 2 2 2 2 2 2 2 2 2 2 2 2
Scatter of Venous
V/Q ratios A A A A A Arterial admixture
■ Figure 2-16 The oxygen cascade. On the left is blood Qs/Qt
P
P
shown the oxygen cascade with PO 2 falling from the level Pao 2 2 2 2 2 2 2 2 2 2
in the ambient air down to the level in the mitochondria.
On the right is a summary of the factors influencing oxy- Blood Haemoglobin
genation at different levels in the cascade. (From Lumb, A. flow concentration
B. [Ed.] [2005]. Nunn’s applied respiratory physiology [6th Q Cell Hb
ed.]. Philadelphia: Elsevier.) 150 E 20 Po 2
Po 2 (mmHg) 100 Dry atmospheric air Air humidified at 37°C A a Arterial blood Mean capilary blood Cytoplasm 15 Po 2 (KPa)
10
50 End-expiratory gas “Ideal” alveolar gas C Mitochondria 5
0 0