Page 617 - ACCCN's Critical Care Nursing
P. 617
594 S P E C I A LT Y P R A C T I C E I N C R I T I C A L C A R E
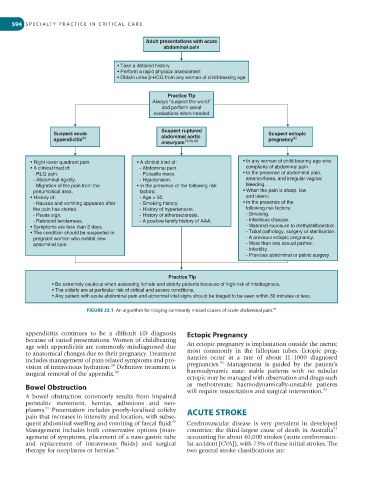
Adult presentations with acute
abdominal pain
• Take a detailed history
• Perform a rapid physical assessment
• Obtain urine β-HCG from any woman of child-bearing age
Practice Tip
Always “suspect the worst”
and perform serial
evaluations when needed
Suspect ruptured
Suspect acute abdominal aortic Suspect ectopic
appendicitis 90 79,88,89 pregnancy 92
aneurysm
• Right lower quadrant pain • A clinical triad of: • In any woman of child bearing-age who
• A clinical triad of: - Abdominal pain. complains of abdominal pain.
- RLQ pain. - Pulsatile mass. • In the presence of abdominal pain,
- Abdominal rigidity. - Hypotension. amenorrhoea, and irregular vaginal
- Migration of the pain from the • In the presence of the following risk bleeding.
periumbilical area. factors: • When the pain is sharp, low
• History of: - Age > 50. and laterol.
- Nausea and vomiting appeared after - Smoking history. • In the presence of the
the pain has started. - History of hypertension. following risk factors:
- Psoas sign. - History of atherosclerosis. - Smoking.
- Rebound tenderness. - A positive family history of AAA. - Infectious disease.
• Symptoms are less than 2 days. - Maternal exposure to diethylstilboestrol.
• The condition should be suspected in - Tubal pathology, surgery or sterilisation.
pregnant women who exhibit new - A previous ectopic pregnancy.
abdominal pain. - More than one sexual partner.
- Infertility.
- Previous abdominal or pelvic surgery.
Practice Tip
• Be extremely cautious when assessing female and elderly patients because of high risk of misdiagnosis.
• The elderly are at particular risk of critical and severe conditions.
• Any patient with acute abdominal pain and abnormal vital signs should be triaged to be seen within 30 minutes or less.
86
FIGURE 22.1 An algorithm for triaging commonly missed causes of acute abdominal pain.
appendicitis continues to be a difficult ED diagnosis Ectopic Pregnancy
because of varied presentations. Women of childbearing
age with appendicitis are commonly misdiagnosed due An ectopic pregnancy is implantation outside the uterus;
to anatomical changes due to their pregnancy. Treatment most commonly in the fallopian tubes. Ectopic preg-
includes management of pain related symptoms and pro- nancies occur at a rate of about 11 : 1000 diagnosed
92
90
vision of intravenous hydration. Definitive treatment is pregnancies. Management is guided by the patient’s
surgical removal of the appendix. 90 haemodynamic state: stable patients with no tubular
ectopic may be managed with observation and drugs such
Bowel Obstruction as methotrexate; haemodynamically-unstable patients
will require resuscitation and surgical intervention.
92
A bowel obstruction commonly results from impaired
peristaltic movement, hernias, adhesions and neo-
91
plasms. Presentation includes poorly-localised colicky ACUTE STROKE
pain that increases in intensity and location, with subse-
91
quent abdominal swelling and vomiting of faecal fluid. Cerebrovascular disease is very prevalent in developed
93
Management includes both conservative options (man- countries; the third-largest cause of death in Australia
agement of symptoms, placement of a naso-gastric tube accounting for about 40,000 strokes (acute cerebrovascu-
and replacement of intravenous fluids) and surgical lar accident [CVA]), with 73% of these initial strokes. The
therapy for neoplasms or hernias. 91 two general stroke classifications are: