Page 1314 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1314
1160 Part VII Hematologic Malignancies
Hypereosinophilia = HE
Familial HE = HE F + Organ
Screen for secondary causes Familial HES = HES F damage
+ Organ Reactive HE = HE R
damage Reactive HES = HES R Positive
Negative Rare syndromes
− Hereditary
Explore underlying cause − Non-hereditary
→Establish the final diagnosis − Mono-organ
Positive Screen for FIP1L1-PDGFRA by FISH or RT-PCR,
and perform cytogenetic analysis for translocations
involving 4q12 (PDGFRA), 5q31-q33 (PDGFRB),
or 8p11-12 (FGFR1)
WHO-based myeloid or
lymphoid neoplasm with HE and Negative
abnormalities of PDGFRA,
PDGFRB or FGFR1 Screen for other molecular markers Abnormal T-cell
and hematologic diseases phenotype ± Th2
cytokine production ?
Define the histopathological and clinical Yes
nature of the underlying neoplasm
→Establish the final diagnosis Other molecular abnormality, clonal No Lymphocyte-variant
eosinophils, and/or increased hypereosinophilia
WHO-defined myeloid marrow blasts (≥5−19%) ?
neoplasm associated HES
with eosinophilia Yes No HE of unknown L + Organ
significance = HE US damage
Chronic eosinophilic
+ Organ leukemia, NOS Idiopathic HES = HES I
damage Neoplastic HES = HES N + Organ
damage
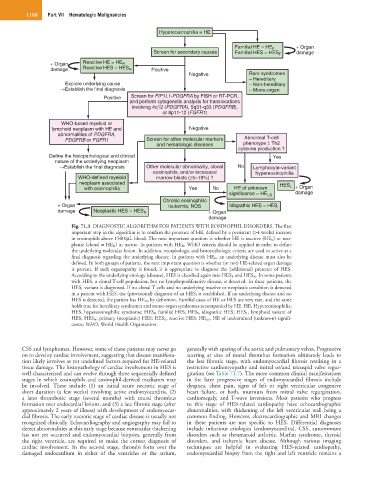
Fig. 71.3 DIAGNOSTIC ALGORITHM FOR PATIENTS WITH EOSINOPHIL DISORDERS. The first
important step in the algorithm is to confirm the presence of HE, defined by a persistent (>4 weeks) increase
in eosinophils above 1500/µL blood. The next important question is whether HE is reactive (HE R ) or neo-
plastic (clonal = HE N ) in nature. In patients with HE N , WHO criteria should be applied in order to define
the underlying molecular lesion. In addition, morphologic and histopathologic criteria are used to arrive at a
final diagnosis regarding the underlying disease. In patients with HE R , an underlying disease must also be
defined. In both groups of patients, the next important question is whether (or not) HE-related organ damage
is present. If such organopathy is found, it is appropriate to diagnose the (additional) presence of HES.
According to the underlying etiology (disease), HES is classified again into HES R and HES N . In some patients
with HES, a clonal T-cell population, but no lymphoproliferative disease, is detected. In these patients, the
HES L variant is diagnosed. If no clonal T cells and no underlying reactive or neoplastic condition is detected
in a patient with HES, the (provisional) diagnosis of an HES I is established. If no underlying disease and no
HES is detected, the patient has HE US by definition. Familial cases of HE or HES are very rare, and the same
holds true for hereditary syndromes and mono-organ syndromes accompanied by HE. HE, Hypereosinophilia;
HES, hypereosinophilic syndrome; HES F , familial HES; HES I , idiopathic HES; HES L , lymphoid variant of
HES; HES N , primary (neoplastic) HES; HES R , reactive HES; HE US , HE of undermined (unknown) signifi-
cance; WHO, World Health Organisation.
CSS and lymphomas. However, some of these patients may never go generally with sparing of the aortic and pulmonary valves. Progressive
on to develop cardiac involvement, suggesting that disease manifesta- scarring at sites of mural thrombus formation ultimately leads to
tion likely involves as yet undefined factors required for HE-related the late fibrotic stage, with endomyocardial fibrosis resulting in a
tissue damage. The histopathology of cardiac involvement in HES is restrictive cardiomyopathy and mitral or/and tricuspid valve regur-
well characterized and can evolve through three sequentially defined gitation (see Table 71.7). The more common clinical manifestations
stages in which eosinophils and eosinophil-derived mediators may in the later progressive stages of endomyocardial fibrosis include
be involved. These include (1) an initial acute necrotic stage of dyspnea, chest pain, signs of left or right ventricular congestive
short duration (a few weeks) involving active endomyocarditis, (2) heart failure, or both, murmurs from mitral valve regurgitation,
a later thrombotic stage (several months) with mural thrombus cardiomegaly, and T-wave inversions. Most patients who progress
formation over endocardial lesions, and (3) a late fibrotic stage (after to this stage of HES-related cardiopathy have echocardiographic
approximately 2 years of illness) with development of endomyocar- abnormalities, with thickening of the left ventricular wall being a
dial fibrosis. The early necrotic stage of cardiac disease is usually not common finding. However, electrocardiographic and MRI changes
recognized clinically. Echocardiography and angiography may fail to in these patients are not specific to HES. Differential diagnoses
detect abnormalities at this early stage because ventricular thickening include infectious etiologies (endomyocarditis), CSS, autoimmune
has not yet occurred and endomyocardial biopsies, generally from disorders such as rheumatoid arthritis, Marfan syndrome, thyroid
the right ventricle, are required to make the correct diagnosis of disorders, and ischemic heart disease. Although various imaging
cardiac involvement. In the second stage, thrombi form over the techniques are helpful in evaluating HES-related cardiopathy,
damaged endocardium in either of the ventricles or the atrium, endomyocardial biopsy from the right and left ventricle remains a