Page 1462 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1462
Chapter 81 Mantle Cell Lymphoma 1299
Naive B cell Early MCL Classical MCL Blastoid MCL
Germline
ATM
CHK2
t(11;14) ATM INK4A/CDK4/RB1
Cyclin D1 CHK2 ARF/MDM2/p53
RB1 p27 Complex High
karyotypes proliferation
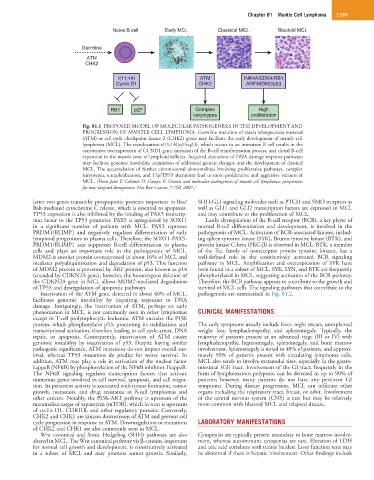
Fig. 81.1 PROPOSED MODEL OF MOLECULAR PATHOGENESIS IN THE DEVELOPMENT AND
PROGRESSION OF MANTLE CELL LYMPHOMA. Germline mutation of ataxia telangiectasia mutated
(ATM) or cell cycle checkpoint kinase 2 (CHK2) genes may facilitate the early development of mantle cell
lymphoma (MCL). The translocation t(11;14)(q13;q23), which occurs in an immature B cell results in the
constitutive overexpression of CCND1 gene, initiation of the B-cell transformation process, and clonal B-cell
expansion in the mantle zone of lymphoid follicles. Acquired alterations of DNA damage response pathways
may facilitate genomic instability, acquisition of additional genetic changes, and the development of classical
MCL. The accumulation of further chromosomal abnormalities involving proliferative pathways, complex
karyotypes, tetraploidization, and 17p/TP53 alterations lead to more proliferative and aggressive variants of
MCL. (From Jares P, Colomer D, Campo E: Genetic and molecular pathogenesis of mantle cell lymphoma: perspectives
for new targeted therapeutics. Nat Rev Cancer 7:750, 2007.)
latter two genes transcribe proapoptotic proteins important in Bax/ SHH-GLI signaling molecules such as PTCH and SMO receptors as
Bak-mediated cytochrome C release, which is essential to apoptosis. well as GLI1 and GLI2 transcription factors are expressed in MCL
TP53 expression is also inhibited by the binding of PAX5 transcrip- and may contribute to the proliferation of MCL.
tion factor to the TP53 promoter. PAX5 is upregulated by SOX11 Lastly, dysregulation of the B-cell receptor (BCR), a key player of
in a significant number of patients with MCL. PAX5 represses normal B-cell differentiation and development, is involved in the
PRDM1/BLIMP1 and negatively regulates differentiation of early pathogenesis of MCL. Activation of BCR-associated kinases, includ-
lymphoid progenitors to plasma cells. Therefore, the SOX11-PAX5- ing spleen tyrosine kinase (SYK), Bruton tyrosine kinase (BTK), and
PRDM1/BLIMP1 axis suppresses B-cell differentiation to plasma protein kinase C-beta (PKC-β) is observed in MCL. BTK, a member
cells and plays an important role in the pathogenesis of MCL. of the Tec family of nonreceptor protein tyrosine kinases, has a
MDM2 is another protein overexpressed in about 16% of MCL and well-defined role in the constitutively activated BCR signaling
mediates polyubiquitination and degradation of p53. This function pathway in MCL. Amplification and overexpression of SYK have
of MDM2 protein is prevented by ARF protein, also known as p14 been found in a subset of MCL. SYK, LYN, and BTK are frequently
(encoded by CDKN2A gene); however, the homozygous deletion of phosphorylated in MCL, suggesting activation of the BCR pathway.
the CDKN2A gene in MCL allows MDM2-mediated degradation Therefore, the BCR pathway appears to contribute to the growth and
of TP53 and dysregulation of apoptotic pathways. survival of MCL cells. The signaling pathways that contribute to the
Inactivation of the ATM gene, detected in about 40% of MCL, pathogenesis are summarized in Fig. 81.2.
facilitates genomic instability by impairing responses to DNA
damage. Intriguingly, the inactivation of ATM, perhaps an early
phenomenon in MCL, is not commonly seen in other lymphomas CLINICAL MANIFESTATIONS
except in T-cell prolymphocytic leukemia. ATM encodes the PI3K
protein, which phosphorylates p53, promoting its stabilization and The early symptoms usually include fever, night sweats, unexplained
transcriptional activation, therefore leading to cell cycle arrest, DNA weight loss, lymphadenopathy, and splenomegaly. Typically, the
repair, or apoptosis. Consequently, inactivation of ATM causes majority of patients present at an advanced stage (III or IV) with
genomic instability by inactivation of p53. Despite having similar lymphadenopathy, hepatomegaly, splenomegaly, and bone marrow
pathogenic significance, ATM mutations do not impact overall sur- involvement. Splenomegaly is noted in 40% of patients, and approxi-
vival, whereas TP53 mutations do predict for worse survival. In mately 50% of patients present with circulating lymphoma cells.
addition, ATM may play a role in activation of the nuclear factor MCL also tends to involve extranodal sites, especially in the gastro-
kappaB (NFκB) by phosphorylation of the NFκB inhibitor, IkappaB. intestinal (GI) tract. Involvement of the GI tract, frequently in the
The NFκB signaling regulates transcription factors that activate form of lymphomatous polyposis, can be detected in up to 90% of
numerous genes involved in cell survival, apoptosis, and cell migra- patients; however, many patients do not have any pertinent GI
tion. Its persistent activity is associated with tumor formation, tumor symptoms. During disease progression, MCL can infiltrate other
growth, metastasis, and drug resistance in B-cell lymphomas and organs including the respiratory tract, breast, or orbit. Involvement
other cancers. Notably, the PI3K-AKT pathway is upstream of the of the central nervous system (CNS) is rare but may be relatively
mammalian target of rapamycin (mTOR), which in turn is upstream more common with blastoid MCL and relapsed disease.
of cyclin D1, CDKI1B, and other regulatory proteins. Conversely,
CHK2 and CHK1 are kinases downstream of ATM and prevent cell
cycle progression in response to ATM. Downregulation or mutations LABORATORY MANIFESTATIONS
of CHK2 and CHK1 are also commonly seen in MCL.
Wnt canonical and Sonic Hedgehog (SHH) pathways are also Cytopenias are typically present secondary to bone marrow involve-
altered in MCL. The Wnt canonical pathway via β-catenin, important ment, whereas autoimmune cytopenias are rare. Elevation of LDH
for normal cell growth and development, is constitutively activated and uric acid correlates with tumor burden. Liver function tests may
in a subset of MCL and may promote tumor growth. Similarly, be abnormal if there is hepatic involvement. Other findings include