Page 1467 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1467
1304 Part VII Hematologic Malignancies
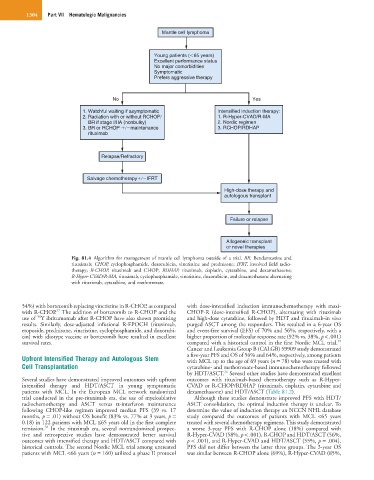
Mantle cell lymphoma
Young patients ( 65 years)
Excellent performance status
No major comorbidities
Symptomatic
Prefers aggressive therapy
No Yes
1. Watchful waiting if asymptomatic Intensified induction therapy:
2. Radiation with or without RCHOP 1. R-Hyper-CVAD/R-MA
BR if stage I/IIA (nonbulky) 2. Nordic regimen
3. BR or RCHOP maintenance 3. RCHOP/RDHAP
rituximab
Relapse/Refractory
Salvage chemotherapy IFRT
High-dose therapy and
autologous transplant
Failure or relapse
Allogeneic transplant
or novel therapies
Fig. 81.4 Algorithm for management of mantle cell lymphoma outside of a trial. BR, Bendamustine and
rituximab; CHOP, cyclophosphamide, doxorubicin, vincristine and prednisone; IFRT, involved field radio-
therapy; R-CHOP, rituximab and CHOP; RDHAP, rituximab, cisplatin, cytarabine, and dexamethasone;
R-Hyper-CVAD/R-MA, rituximab, cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating
with rituximab, cytarabine, and methotrexate.
54%) with bortezomib replacing vincristine in R-CHOP, as compared with dose-intensified induction immunochemotherapy with maxi-
37
with R-CHOP. The addition of bortezomib to R-CHOP and the CHOP-R (dose-intensified R-CHOP), alternating with rituximab
90
use of Y ibritumomab after R-CHOP have also shown promising and high-dose cytarabine, followed by HDT and rituximab-in vivo
results. Similarly, dose-adjusted infusional R-EPOCH (rituximab, purged ASCT among the responders. This resulted in a 6-year OS
etoposide, prednisone, vincristine, cyclophosphamide, and doxorubi- and event-free survival (EFS) of 70% and 56%, respectively, with a
cin) with idiotype vaccine or bortezomib have resulted in excellent higher proportion of molecular response rate (92% vs. 38%, p < .001)
39
survival rates. compared with a historical control in the first Nordic MCL trial.
Cancer and Leukemia Group B (CALGB) 59909 study demonstrated
Upfront Intensified Therapy and Autologous Stem a five-year PFS and OS of 56% and 64%, respectively, among patients
with MCL up to the age of 69 years (n = 78) who were treated with
Cell Transplantation cytarabine- and methotrexate-based immunochemotherapy followed
24
by HDT/ASCT. Several other studies have demonstrated excellent
Several studies have demonstrated improved outcomes with upfront outcomes with rituximab-based chemotherapy such as R-Hyper-
intensified therapy and HDT/ASCT in young symptomatic CVAD or R-CHOP/RDHAP (rituximab, cisplatin, cytarabine and
patients with MCL. In the European MCL network randomized dexamethasone) and HDT/ASCT (Table 81.2).
trial conducted in the pre-rituximab era, the use of myeloablative Although these studies demonstrate improved PFS with HDT/
radiochemotherapy and ASCT versus α-interferon maintenance ASCT consolidation, the optimal induction therapy is unclear. To
following CHOP-like regimen improved median PFS (39 vs. 17 determine the value of induction therapy an NCCN NHL database
months, p = .01) without OS benefit (83% vs. 77% at 3 years, p = study compared the outcomes of patients with MCL <65 years
0.18) in 122 patients with MCL ≤65 years old in the first complete treated with several chemotherapy regimens. This study demonstrated
38
remission. In the rituximab era, several nonrandomized prospec- a worse 3-year PFS with R-CHOP alone (18%) compared with
tive and retrospective studies have demonstrated better survival R-Hyper-CVAD (58%, p < .001), R-CHOP and HDT/ASCT (56%,
outcomes with intensified therapy and HDT/ASCT compared with p < .001), and R-Hyper-CVAD and HDT/ASCT (55%, p = .004).
historical controls. The second Nordic MCL trial among untreated PFS did not differ between the latter three groups. The 3-year OS
patients with MCL <66 years (n = 160) utilized a phase II protocol was similar between R-CHOP alone (69%), R-Hyper-CVAD (85%,