Page 1503 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1503
Chapter 84 Malignant Lymphomas in Childhood 1335
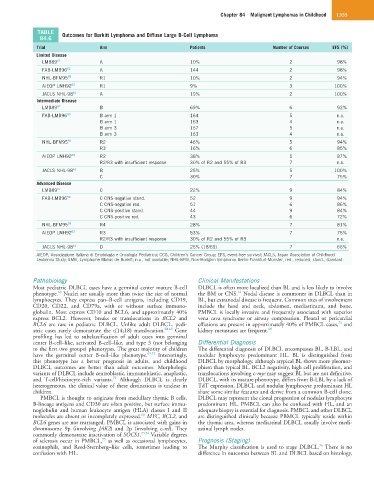
TABLE Outcomes for Burkitt Lymphoma and Diffuse Large B-Cell Lymphoma
84.6
Trial Arm Patients Number of Courses EFS (%)
Limited Disease
LMB89 57 A 10% 2 98%
FAB-LMB96 62 A 144 2 98%
NHL-BFM95 59 R1 10% 2 94%
AIEOP LNH92 63 R1 9% 3 100%
JACLS NHL-98 61 A 19% 2 100%
Intermediate Disease
LMB89 57 B 69% 6 92%
FAB-LMB96 60 B arm 1 164 5 n.a.
B arm 1 163 4 n.a.
B arm 3 167 5 n.a.
B arm 3 163 4 n.a.
NHL-BFM95 59 R2 46% 5 94%
R3 16% 6 85%
AIEOP LNH92 63 R2 38% 5 87%
R2/R3 with insufficient response 30% of R2 and 55% of R3 7 n.a.
JACLS NHL-98 61 B 25% 5 100%
C 30% 7 75%
Advanced Disease
LMB89 57 C 22% 9 84%
FAB-LMB96 58 C CNS-negative stand. 52 9 94%
C CNS-negative red. 51 6 86%
C CNS-positive stand. 44 9 84%
C CNS-positive red. 43 6 72%
NHL-BFM95 59 R4 28% 7 81%
AIEOP LNH92 63 R3 53% 7 75%
R2/R3 with insufficient response 30% of R2 and 55% of R3 n.a.
JACLS NHL-98 61 D 26% (18/69) 7 66%
AIEOP, Associazione Italiana di Ematologia e Oncologia Pediatrica; CCG, Children’s Cancer Group; EFS, event-free survival; JACLS, Japan Association of Childhood
Leukemia Study; LMB, Lymphome Malins de Burkitt; n.a., not available; NHL-BFM, Non-Hodgkin lymphoma Berlin-Frankfurt-Münster; red., reduced; stand., standard.
Pathobiology Clinical Manifestations
Most pediatric DLBCL cases have a germinal center mature B-cell DLBCL is often more localized than BL and is less likely to involve
24
69
phenotype. Nuclei are usually more than twice the size of normal the BM or CNS. Nodal disease is commoner in DLBCL than in
lymphocytes. They express pan–B-cell antigens, including CD19, BL, but extranodal disease is frequent. Common sites of involvement
CD20, CD22, and CD79a, with or without surface immuno- include the head and neck, abdomen, mediastinum, and bone.
globulin. Most express CD10 and BCL6, and approximately 40% PMBCL is locally invasive and frequently associated with superior
express BCL2. However, breaks or translocations in BCL2 and vena cava syndrome or airway compression. Pleural or pericardial
75
BCL6 are rare in pediatric DLBCL. Unlike adult DLBCL, pedi- effusions are present in approximately 40% of PMBCL cases, and
atric cases rarely demonstrate the t(14;18) translocation. 68,69 Gene kidney metastases are frequent. 68
profiling has led to subclassification of adult cases into germinal
center B-cell–like, activated B-cell–like, and type 3 (not belonging Differential Diagnosis
to the first two groups) phenotypes. The great majority of children The differential diagnosis of DLBCL encompasses BL, B-LBL, and
have the germinal center B-cell–like phenotype. 69,71 Interestingly, nodular lymphocyte predominant HL. BL is distinguished from
this phenotype has a better prognosis in adults, and childhood DLBCL by morphology, although atypical BL shows more pleomor-
DLBCL outcomes are better than adult outcomes. Morphologic phism than typical BL. BCL2 negativity, high cell proliferation, and
variants of DLBCL include centroblastic, immunoblastic, anaplastic, translocations involving c-myc may suggest BL but are not definitive.
72
and T-cell/histiocyte-rich variants. Although DLBCL is clearly DLBCL, with its mature phenotype, differs from B-LBL by a lack of
heterogeneous, the clinical value of these distinctions is unclear in TdT expression. DLBCL and nodular lymphocyte predominant HL
children. share some similar features and derive from a common B-cell clone.
PMBCL is thought to originate from medullary thymic B cells. DLBCL may represent the clonal progression of nodular lymphocyte
B-lineage antigens and CD30 are often positive, but surface immu- predominant HL. PMBCL can also be confused with HL, and an
noglobulin and human leukocyte antigen (HLA) classes I and II adequate biopsy is essential for diagnosis. PMBCL and other DLBCL
68
molecules are absent or incompletely expressed. MYC, BCL2, and are distinguished clinically because PBMCL typically reside within
BCL6 genes are not rearranged. PMBCL is associated with gains in the thymic area, whereas mediastinal DLBCL usually involve medi-
chromosome 9p (involving JAK2) and 2p (involving c-rel). They astinal lymph nodes.
commonly demonstrate inactivation of SOCS1. 73,74 Variable degrees
75
of sclerosis occur in PMBCL, as well as occasional lymphocytes, Prognosis (Staging)
76
eosinophils, and Reed-Sternberg–like cells, sometimes leading to The Murphy classification is used to stage DLBCL. There is no
confusion with HL. difference in outcomes between BL and DLBCL based on histology,