Page 1797 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1797
Chapter 104 Indications and Outcomes of Allogeneic Hematopoietic Cell Transplantation for Hematologic Malignancies in Adults 1601
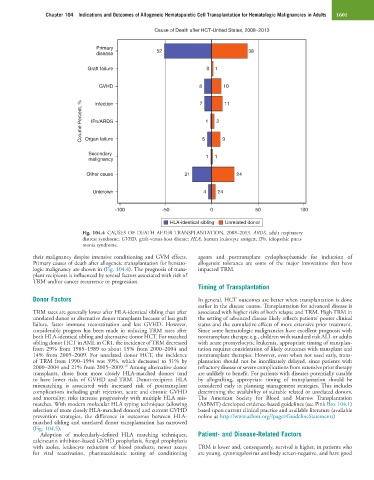
Cause of Death after HCT-United States, 2008−2013
Primary 52
disease 38
Graft failure 0 1
GVHD 8 7 10
Colume Percent, % IPn/ARDS 1 2
11
Infection
Organ failure
Secondary 5 1 9
malignancy 1
Other cause 21 24
Unknown 4 24
-100 -50 0 50 100
HLA-identical sibling Unrelated donor
Fig. 104.4 CAUSES OF DEATH AFTER TRANSPLANTATION, 2008–2013. ARDS, adult respiratory
distress syndrome; GVHD, graft-versus-host disease; HLA, human leukocyte antigen; IPn, idiopathic pneu-
monia syndrome.
their malignancy despite intensive conditioning and GVM effects. agents and posttransplant cyclophosphamide for induction of
Primary causes of death after allogeneic transplantation for hemato- allogeneic tolerance are some of the major innovations that have
logic malignancy are shown in (Fig. 104.4). The prognosis of trans- impacted TRM.
plant recipients is influenced by several factors associated with risk of
TRM and/or cancer recurrence or progression.
Timing of Transplantation
Donor Factors In general, HCT outcomes are better when transplantation is done
earlier in the disease course. Transplantation for advanced disease is
TRM rates are generally lower after HLA-identical sibling than after associated with higher risks of both relapse and TRM. High TRM in
unrelated donor or alternative donor transplants because of less graft the setting of advanced disease likely reflects patients’ poorer clinical
failure, faster immune reconstitution and less GVHD. However, status and the cumulative effects of more extensive prior treatment.
considerable progress has been made in reducing TRM rates after Since some hematologic malignancies have excellent prognosis with
both HLA-identical sibling and alternative donor HCT. For matched nontransplant therapy, e.g., children with standard risk ALL or adults
sibling donor HCT in AML in CR1, the incidence of TRM decreased with acute promyelocytic leukemia, appropriate timing of transplan-
from 29% from 1985–1989 to about 15% from 2000–2004 and tation requires consideration of likely outcomes with transplant and
14% from 2005–2009. For unrelated donor HCT, the incidence nontransplant therapies. However, even when not used early, trans-
of TRM from 1990–1994 was 39%, which decreased to 31% by plantation should not be inordinately delayed, since patients with
18
2000–2004 and 21% from 2005–2009. Among alternative donor refractory disease or severe complications from extensive prior therapy
transplants, those from more closely HLA-matched donors tend are unlikely to benefit. For patients with diseases potentially curable
to have lower risks of GVHD and TRM. Donor-recipient HLA by allografting, appropriate timing of transplantation should be
mismatching is associated with increased risk of posttransplant considered early in planning management strategies. This includes
complications including graft rejection, acute and chronic GVHD determining the availability of suitable related or unrelated donors.
and mortality; risks increase progressively with multiple HLA mis- The American Society for Blood and Marrow Transplantation
matches. With modern molecular HLA typing techniques (allowing (ASBMT) developed evidence-based guidelines (see Pink Box 104.1)
selection of more closely HLA-matched donors) and current GVHD based upon current clinical practice and available literature (available
prevention strategies, the difference in outcomes between HLA- online at http://www.asbmt.org/?page=GuidelineStatements)
matched sibling and unrelated donor transplantation has narrowed
(Fig. 104.5).
Adoption of molecularly-defined HLA matching techniques, Patient- and Disease-Related Factors
calcineurin inhibitor–based GVHD prophylaxis, fungal prophylaxis
with azoles, leukocyte reduction of blood products, newer assays TRM is lower and, consequently, survival is higher, in patients who
for viral reactivation, pharmacokinetic testing of conditioning are young, cytomegalovirus antibody screen-negative, and have good