Page 1889 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1889
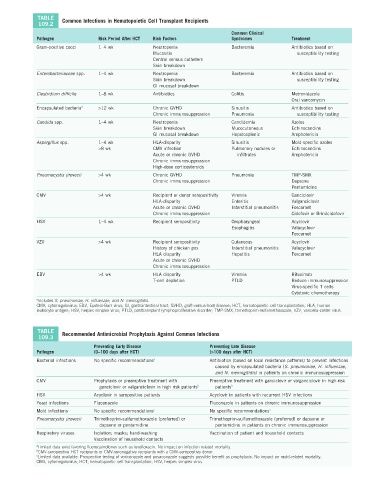
TABLE Common Infections in Hematopoietic Cell Transplant Recipients
109.2
Common Clinical
Pathogen Risk Period After HCT Risk Factors Syndromes Treatment
Gram-positive cocci 1–4 wk Neutropenia Bacteremia Antibiotics based on
Mucositis susceptibility testing
Central venous catheters
Skin breakdown
Enterobacteriaceae spp. 1–4 wk Neutropenia Bacteremia Antibiotics based on
Skin breakdown susceptibility testing
GI mucosal breakdown
Clostridium difficile 1–8 wk Antibiotics Colitis Metronidazole
Oral vancomycin
Encapsulated bacteria a >12 wk Chronic GVHD Sinusitis Antibiotics based on
Chronic immunosuppression Pneumonia susceptibility testing
Candida spp. 1–4 wk Neutropenia Candidemia Azoles
Skin breakdown Mucocutaneous Echinocandins
GI mucosal breakdown Hepatosplenic Amphotericin
Aspergillus spp. 1–4 wk HLA-disparity Sinusitis Mold-specific azoles
>8 wk CMV infection Pulmonary nodules or Echinocandins
Acute or chronic GVHD infiltrates Amphotericin
Chronic immunosuppression
High-dose corticosteroids
Pneumocystis jirovecii >4 wk Chronic GVHD Pneumonia TMP-SMX
Chronic immunosuppression Dapsone
Pentamidine
CMV >4 wk Recipient or donor seropositivity Viremia Ganciclovir
HLA-disparity Enteritis Valganciclovir
Acute or chronic GVHD Interstitial pneumonitis Foscarnet
Chronic immunosuppression Cidofovir or Brindcidofovir
HSV 1–4 wk Recipient seropositivity Oropharyngeal Acyclovir
Esophagitis Valacyclovir
Foscarnet
VZV >4 wk Recipient seropositivity Cutaneous Acyclovir
History of chicken pox Interstitial pneumonitis Valacyclovir
HLA disparity Hepatitis Foscarnet
Acute or chronic GVHD
Chronic immunosuppression
EBV >4 wk HLA disparity Viremia Rituximab
T-cell depletion PTLD Reduce immunosuppression
Virus-specific T cells
Cytotoxic chemotherapy
a Includes S. pneumoniae, H. influenzae, and N. meningitidis.
CMV, cytomegalovirus; EBV, Epstein-Barr virus; GI, gastrointestinal tract; GVHD, graft-versus-host disease; HCT, hematopoietic cell transplantation; HLA, human
leukocyte antigen; HSV, herpes simplex virus; PTLD, posttransplant lymphoproliferative disorder; TMP-SMX, trimethoprim-sulfamethoxazole; VZV, varicella-zoster virus.
TABLE Recommended Antimicrobial Prophylaxis Against Common Infections
109.3
Preventing Early Disease Preventing Late Disease
Pathogen (0–100 days after HCT) (>100 days after HCT)
Bacterial infections No specific recommendations a Antibiotics (based on local resistance patterns) to prevent infections
caused by encapsulated bacteria (S. pneumoniae, H. influenzae,
and N. meningitidis) in patients on chronic immunosuppression
CMV Prophylaxis or preemptive treatment with Preemptive treatment with ganciclovir or valganciclovir in high-risk
ganciclovir or valganciclovir in high risk patients b patients b
HSV Acyclovir in seropositive patients Acyclovir in patients with recurrent HSV infections
Yeast infections Fluconazole Fluconazole in patients on chronic immunosuppression
Mold infections No specific recommendations c No specific recommendations a
Pneumocystis jirovecii Trimethoprim-sulfamethoxazole (preferred) or Trimethoprim-sulfamethoxazole (preferred) or dapsone or
dapsone or pentamidine pentamidine in patients on chronic immunosuppression
Respiratory viruses Isolation; masks; hand-washing Vaccination of patient and household contacts
Vaccination of household contacts
a Limited data exist favoring fluoroquinolones such as levofloxacin. No impact on infection-related mortality.
b CMV-seropositive HCT recipients or CMV-seronegative recipients with a CMV-seropositive donor.
c Limited data available. Prospective testing of voriconazole and posaconazole suggests possible benefit as prophylaxis. No impact on mold-related mortality.
CMV, cytomegalovirus; HCT, hematopoietic cell transplantation; HSV, herpes simplex virus.