Page 1972 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 1972
1746 Part XI Transfusion Medicine
100 rate or postoperative liver function tests between those who received
plasma from those who did not. Two other studies showed a poor
correlation between number of plasma transfusions, PT and PTT
Coagulation factors (%) 50 Zone of normal hemostasis plantation. Lastly, a randomized control trial revealed that intranasal
values, and number of RBCs transfusions needed during liver trans-
(physiologic reserve)
desmopressin was both less expensive and as effective as plasma
transfusions for liver disease patients with an INR between 2.0 and
3.0 undergoing minor surgery.
As a result of these studies, authorities now suggest that the use
30
Zone of
therapeutic
The transfusion of plasma in these patients should be guided by a
anticoagulation of plasma be more limited in liver disease and hepatectomy patients.
combination of clinical assessment, the evidence and degree of bleed-
ing, and by coagulation test results. Plasma products are currently not
recommended prophylactically before a surgical challenge or liver
PT (sec) 12 13 14 15 16 17 18 19 20 21 22
biopsy in these patients. However, as noted previously, plasma trans-
INR 1.0 1.3 1.7 2.0 2.2 3.0 fusions may be considered when the PT/PTT is greater than 1.5 to
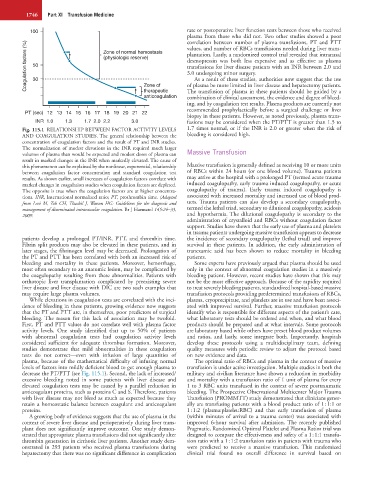
Fig. 115.1 RELATIONSHIP BETWEEN FACTOR ACTIVITY LEVELS 1.7 times normal, or if the INR is 2.0 or greater when the risk of
AND COAGULATION STUDIES. The general relationship between the bleeding is considered high.
concentration of coagulation factors and the result of PT and INR studies.
The normalization of modest elevations in the INR required much larger
volumes of plasma than would be expected and modest doses of plasma can Massive Transfusion
result in marked changes in the INR when markedly elevated. The cause of
this phenomenon can be explained by the nonlinear, exponential, relationship Massive transfusion is generally defined as receiving 10 or more units
between coagulation factor concentration and standard coagulation test of RBCs within 24 hours (or one blood volume). Trauma patients
results. As shown earlier, small increases of coagulation factors correlate with may arrive at the hospital with a prolonged PT (termed acute trauma
marked changes in coagulation studies when coagulation factors are depleted. induced coagulopathy, early trauma induced coagulopathy, or acute
The opposite is true when the coagulation factors are at higher concentra- coagulopathy of trauma). Early trauma induced coagulopathy is
tions. INR, International normalized ratio; PT, prothrombin time. (Adapted associated with increased mortality and increased use of blood prod-
from Levi M, Toh CH, Thachil J, Watson HG: Guidelines for the diagnosis and ucts. Trauma patients can also develop a secondary coagulopathy,
management of disseminated intravascular coagulation. Br J Haematol 145:24–33, termed the lethal triad, secondary to dilutional coagulopathy, acidosis
2009. and hypothermia. The dilutional coagulopathy is secondary to the
administration of crystalloid and RBCs without coagulation factor
support. Studies have shown that the early use of plasma and platelets
in trauma patients undergoing massive transfusion appears to decrease
patients develop a prolonged PT/INR, PTT, and thrombin time. the incidence of secondary coagulopathy (lethal triad) and improve
Fibrin split products may also be elevated in these patients, and in survival in these patients. In addition, the early administration of
later stages, the fibrinogen level may be decreased. Prolongation of tranexamic acid has been shown to reduce mortality in bleeding
the PT and PTT has been correlated with both an increased risk of patients.
bleeding and mortality in these patients. Moreover, hemorrhage, Some experts have previously argued that plasma should be used
most often secondary to an anatomic lesion, may be complicated by only in the context of abnormal coagulation studies in a massively
the coagulopathy resulting from these abnormalities. Patients with bleeding patient. However, recent studies have shown that this may
orthotopic liver transplantation complicated by preexisting severe not be the most effective approach. Because of the rapidity required
liver disease and liver disease with DIC are two such examples that to treat severely bleeding patients, standardized hospital-based massive
may require large plasma volumes. transfusion protocols providing predetermined transfusions of RBCs,
While elevations in coagulation tests are correlated with the inci- plasma, cryoprecipitate, and platelets are in use and have been associ-
dence of bleeding in these patients, growing evidence now suggests ated with improved survival. Further, massive transfusion protocols
that the PT and PTT are, in themselves, poor predictors of surgical identify who is responsible for different aspects of the patient’s care,
bleeding. The reason for this lack of association may be twofold. what laboratory tests should be ordered and when, and what blood
First, PT and PTT values do not correlate well with plasma factor products should be prepared and at what intervals. Some protocols
activity levels. One study identified that up to 50% of patients are laboratory based while others have preset blood product volumes
with abnormal coagulation tests had coagulation activity levels and ratios, and lastly, some integrate both. Importantly, hospitals
considered sufficient for adequate thrombus formation. Moreover, develop these protocols using a multidisciplinary team, defining
studies demonstrate that mild abnormalities in these coagulation quality measures with periodic review to adjust the protocol based
tests do not correct—even with infusion of large quantities of on new evidence and data.
plasma, because of the mathematical difficulty of infusing normal The optimal ratio of RBCs and plasma in the context of massive
levels of factors into mildly deficient blood to get enough plasma to transfusion is under active investigation. Multiple studies in both the
decrease the PT/PTT (see Fig. 115.1). Second, the lack of increased/ military and civilian literature have shown a reduction in morbidity
excessive bleeding noted in some patients with liver disease and and mortality with a transfusion ratio of 1 unit of plasma for every
elevated coagulation tests may be caused by a parallel reduction in 1 to 3 RBC units transfused in the context of severe posttraumatic
anticoagulant proteins, such as proteins C and S. Therefore, patients bleeding. The Prospective Observational Multicenter Major Trauma
with liver disease may not bleed as much as expected because they Transfusion (PROMMTT) study demonstrated that clinicians gener-
retain a homeostatic balance between coagulant and anticoagulant ally are transfusing patients with a blood product ratio of 1 : 1:1 or
proteins. 1 : 1:2 (plasma:platelet:RBC) and that early transfusion of plasma
A growing body of evidence suggests that the use of plasma in the (within minutes of arrival to a trauma center) was associated with
context of severe liver disease and perioperatively during liver trans- improved 6-hour survival after admission. The recently published
plant does not significantly improve outcome. One study demon- Pragmatic, Randomized Optimal Platelet and Plasma Ratios trial was
strated that appropriate plasma transfusions did not significantly alter designed to compare the effectiveness and safety of a 1 : 1:1 transfu-
thrombin generation in cirrhotic liver patients. Another study dem- sion ratio with a 1 : 1:2 transfusion ratio in patients with trauma who
onstrated in 293 patients who received plasma transfusions during were predicted to receive a massive transfusion. This randomized
hepatectomy that there was no significant difference in complication clinical trial found no overall difference in survival based on