Page 2323 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2323
Chapter 139 Disseminated Intravascular Coagulation 2065
Endothelial polyphosphates, and glycosaminoglycans, are potential activators of
cells the contact pathway. Studies in patients with suspected DIC have
identified elevated levels of markers of activation of the contact
Cytokines Inflammatory cells system. In patients with meningococcal septicemia, there was a nega-
tive correlation between plasma factor XII levels and factor XIIa–C1
inhibitor complexes. Although this finding implies consumption of
factor XII, and subsequent downstream activation of factor XI, an
Tissue factor alternative explanation is that there is a negative acute phase effect
expression
with reduced synthesis of factor XII, in conjunction with thrombin-
mediated activation of factor XI.
Impairment of However, blockade of the contact system with a factor XIIa–
physiologic directed antibody failed to prevent DIC in a balloon model of
anticoagulant Escherichia coli sepsis, but diminished development of lethal hypoten-
mechanisms
sion. These findings provide reasonable support for the current view
that the contact pathway does not contribute to DIC, but may play
important roles in proinflammatory mechanisms related to vascular
Inhibition of permeability, vascular proliferation (kininogen induces smooth
11
fibrinolysis muscle cell proliferation), and enhancement of fibrinolysis.
due to high
levels of PAI-1
Cytokines and Other Amplification Pathways
Activation of blood coagulation requires several cofactors. For devel-
MICROVASCULAR THROMBOSIS AND opment of DIC, the surfaces of cell remnants or intact cells, inflam-
MODULATION OF INFLAMMATION matory mediators, and coagulation proteins are required. The
stimulus for activation depends on the underlying disease and may
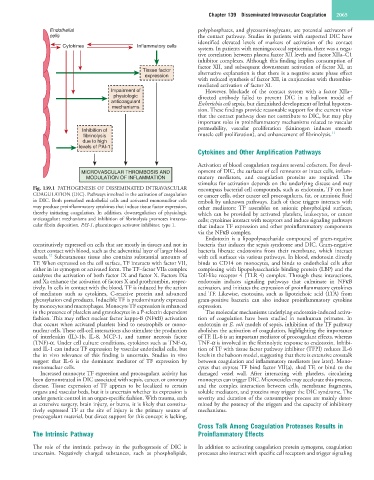
Fig. 139.1 PATHOGENESIS OF DISSEMINATED INTRAVASCULAR encompass bacterial cell compounds, such as endotoxin, TF on host
COAGULATION (DIC). Pathways involved in the activation of coagulation or cancer cells, other cancer cell procoagulants, fat, or amniotic fluid
in DIC. Both perturbed endothelial cells and activated mononuclear cells emboli by unknown pathways. Each of these triggers interacts with
may produce proinflammatory cytokines that induce tissue factor expression, other mediators: TF assembles on anionic phospholipid surfaces,
thereby initiating coagulation. In addition, downregulation of physiologic which can be provided by activated platelets, leukocytes, or cancer
anticoagulant mechanisms and inhibition of fibrinolysis promotes intravas- cells; cytokines interact with receptors and induce signaling pathways
cular fibrin deposition. PAI-1, plasminogen activator inhibitor, type 1. that induce TF expression and other proinflammatory components
via the NFκB complex.
Endotoxin is a lipopolysaccharide compound of gram-negative
constitutively expressed on cells that are mostly in tissues and not in bacteria that induces the sepsis syndrome and DIC. Gram-negative
direct contact with blood, such as the adventitial layer of larger blood bacteria liberate endotoxins from their membrane, which interact
12
vessels. Subcutaneous tissue also contains substantial amounts of with cell surfaces via various pathways. In blood, endotoxin directly
TF. When expressed on the cell surface, TF interacts with factor VII, binds to CD14 on monocytes, and binds to endothelial cells after
either in its zymogen or activated form. The TF–factor VIIa complex complexing with lipopolysaccharide binding protein (LBP) and the
catalyzes the activation of both factor IX and factor X. Factors IXa Toll-like receptor 4 (TLR 4) complex. Through these interactions,
and Xa enhance the activation of factors X and prothrombin, respec- endotoxin induces signaling pathways that culminate in NFκB
tively. In cells in contact with the blood, TF is induced by the action activation, and initiates the expression of proinflammatory cytokines
of mediators such as cytokines, C-reactive protein and advanced and TF. Likewise, exotoxins, such as lipoteichoic acid (LTA) from
glycosylation end products. Inducible TF is predominantly expressed gram-positive bacteria can also induce proinflammatory cytokine
by monocytes and macrophages. Monocyte TF expression is enhanced expression.
in the presence of platelets and granulocytes in a P-selectin dependent The molecular mechanisms underlying endotoxin-induced activa-
fashion. This may reflect nuclear factor kappa-B (NFκB) activation tion of coagulation have been studied in nonhuman primates. In
that occurs when activated platelets bind to neutrophils or mono- endotoxin or E. coli models of sepsis, inhibition of the TF pathway
nuclear cells. These cell-cell interactions also stimulate the production abolishes the activation of coagulation, highlighting the importance
of interleukin (IL)-1b, IL-8, MCP-1, and tumor necrosis factor of TF. IL-6 is an important mediator of procoagulant effects, whereas
(TNF)-α. Under cell culture conditions, cytokines such as TNF-α, TNF-α is involved in the fibrinolytic response to endotoxin. Inhibi-
and IL-1 can induce TF expression by vascular endothelial cells, but tion of TF with tissue factor pathway inhibitor (TFPI) reduces IL-6
the in vivo relevance of this finding is uncertain. Studies in vivo levels in the baboon model, suggesting that there is extensive crosstalk
suggest that IL-6 is the dominant mediator of TF expression by between coagulation and inflammatory mediators (see later). Mono-
mononuclear cells. cytes that express TF bind factor VII(a), shed TF, or bind to the
Increased monocyte TF expression and procoagulant activity has damaged vessel wall. After interacting with platelets, circulating
been demonstrated in DIC associated with sepsis, cancer, or coronary monocytes can trigger DIC. Microvesicles may accelerate this process,
disease. Tissue expression of TF appears to be localized to certain and the complex interaction between cells, membrane fragments,
organs and vascular beds, but it is uncertain whether its expression is soluble mediators, and proteins may trigger the DIC syndrome. The
under genetic control in an organ-specific fashion. With trauma, such severity and duration of the consumptive process are mainly deter-
as extensive surgery, brain injury, or burns, it is likely that constitu- mined by the potency of the triggers and the capacity of inhibitory
tively expressed TF at the site of injury is the primary source of mechanisms.
procoagulant material, but direct support for this concept is lacking.
Cross Talk Among Coagulation Proteases Results in
The Intrinsic Pathway Proinflammatory Effects
The role of the intrinsic pathway in the pathogenesis of DIC is In addition to activating coagulation protein zymogens, coagulation
uncertain. Negatively charged substances, such as phospholipids, proteases also interact with specific cell receptors and trigger signaling