Page 2454 - Hematology_ Basic Principles and Practice ( PDFDrive )
P. 2454
2192 Part XII Hemostasis and Thrombosis
On physical examination, the location and characteristics of maternal antibody or drug, and platelet size. A classification of
bleeding (e.g., procedural, mucosal, cutaneous, intraventricular), neonatal thrombocytopenia is provided in Table 150.3. Thrombocy-
9
12
whether diffuse or localized, in addition to the general appearance of topenia is defined as a platelet count less than 150 × 10 /L. Platelet
9
the baby as sick or well, will help to identify the underlying etiology counts in the range of 100 to 150 × 10 /L are common in healthy
of the hemorrhage. In ill-appearing newborns, disseminated intravas- neonates; these mostly reflect transient thrombocytopenia and require
cular coagulation (DIC) or liver disease may result in acquired factor no further investigation unless there is a further decrease in the count.
9
deficiencies. These disorders tend to present with diffuse bleeding. More severe thrombocytopenia (platelet count <50 × 10 /L) in
Well-appearing newborns are more likely to have localized bleeding neonates rarely manifests with bleeding, particularly in the absence
or ecchymoses because of thrombocytopenia from a transplacental of maternal antiplatelet antibodies. The estimated prevalence of
antibody, vitamin K deficiency, or a rare inherited factor deficiency. thrombocytopenia is in the range of 1% to 5% of all newborns. The
Laboratory evaluation of the hemorrhage in newborns should prevalence of thrombocytopenia increases to 22% to 35% in neonates
include sepsis evaluation and determination of the platelet count, PT, admitted to the neonatal intensive care unit (NICU), with the rates
aPTT, thrombin time, and fibrinogen concentration. If the test increasing with decreasing gestational age. With severe thrombocyto-
results are normal, bleeding neonates or infants should be assessed penia, platelet transfusion may be necessary to treat or decrease the
for FXIII and α 2AP activity. Deficiencies of FXIII, α 2AP, or PAI-1 risk of bleeding.
are not detected with routine screening, and specific testing is needed Causes of neonatal thrombocytopenia include decreased platelet
if deficiencies are suspected. The approach to laboratory screening is production, increased platelet consumption, and/or hypersplenism
summarized in Fig. 150.1, which has been modified from Blanchette (see Chapters 131 and 132). Other contributing factors include infec-
10
and Rand. Platelet function should be evaluated when primary tion, placental insufficiency, genetic disorders, medications, DIC, or
11
hemostatic defects are suspected. In male infants with a family immune deficiency. In well-appearing newborns, thrombocytopenia
history of hemophilia or when hemophilia is suspected, the levels of is usually immune mediated and related to maternal transplacental
FVIII and FIX should be determined, regardless of the degree of immunoglobulin G antibodies or drugs (e.g., quinine, hydralazine,
aPTT prolongation. thiazides, tolbutamide). In sick newborns, platelet destruction is often
related to infection, DIC, extracorporeal membrane oxygenation
(ECMO), thrombosis, or mechanical ventilation for hyaline mem-
Neonatal Thrombocytopenia brane disease. Large-vessel thrombosis can also lead to thrombocyto-
penia, as can specific syndromes, such as renal vein thrombosis (RVT),
The following factors are important to consider when evaluating necrotizing enterocolitis, or vascular anomalies (Kasabach-Merritt
neonates with thrombocytopenia: congenital or acquired, sick or well, syndrome). Platelet production can be impaired with hypoxic-ischemic
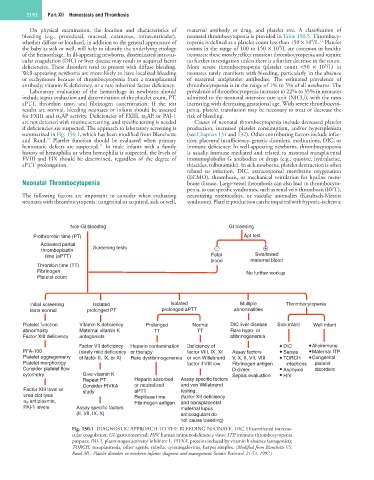
Non-GI bleeding GI bleeding
Prothrombin time (PT) Apt test
Activated partial
thromboplastin Screening tests - +
time (aPTT) Fetal Swallowed
blood maternal blood
Thrombin time (TT)
Fibrinogen No further workup
Platelet count
Initial screening Isolated Isolated Multiple Thrombocytopenia
tests normal prolonged PT prolonged aPTT abnormalities
Platelet function Vitamin K deficiency Prolonged Normal DIC liver disease Sick infant Well infant
abnormality Maternal vitamin K TT TT Rare hypo- or
Factor XIII deficiency antagonists afibrinogenemia
Factor VII deficiency Heparin contamination Deficiency of DIC Alloimmune
PFA-100 (rarely mild deficiency or therapy factor VIII, IX, XI Assay factors Sepsis Maternal ITP
Platelet aggregometry of factor II, IX, or X) Rare dysfibrinogenemia or von Willebrand V, X, II, VII, VIII TORCH Congenital
Platelet morphology factor if VIII low Fibrinogen antigen infections platelet
Consider platelet flow D-dimer Asphyxia disorders
cytometry Give vitamin K Sepsis evaluation HIV
Repeat PT Heparin absorbed Assay specific factors
Consider PIVKA or neutralized and von Willebrand
Factor XIII level or study aPTT testing.
urea clot lysis Reptilase time (factor XII deficiency
α 2 antiplasmin, Fibrinogen antigen and transplacental
PAI-1 levels Assay specific factors maternal lupus
(II, VII, IX, X) anticoagulant do
not cause bleeding)
Fig. 150.1 DIAGNOSTIC APPROACH TO THE BLEEDING NEONATE. DIC, Disseminated intravas-
cular coagulation; GI, gastrointestinal; HIV, human immunodeficiency virus; ITP, immune thrombocytopenia
purpura; PAI-1, plasminogen activator inhibitor 1; PIVKA, proteins induced by vitamin k absence (antagonist);
TORCH, toxoplasmosis, other agents, rubella, cytomegalovirus, herpes simplex. (Modified from Blanchette VS,
Rand ML: Platelet disorders in newborn infants: diagnosis and management. Semin Perinatol 21:53, 1997.)