Page 1814 - Williams Hematology ( PDFDrive )
P. 1814
1788 Part XI: Malignant Lymphoid Diseases Chapter 109: Macroglobulinemia 1789
TABLE 109–2. Physicochemical and Immunological Properties of the Monoclonal Immunoglobulin M Protein in
Waldenström’s Macroglobulinemia
Properties of IgM Monoclonal Protein Diagnostic Condition Clinical Manifestations
Pentameric structure Hyperviscosity Headaches, blurred vision, epistaxis, retinal hemorrhages,
leg cramps, impaired mentation, intracranial hemorrhage
Precipitation on cooling Cryoglobulinemia (type I) Raynaud phenomenon, acrocyanosis, ulcers, purpura, cold
urticaria
Autoantibody activity to myelin-associated Peripheral neuropathies Sensorimotor neuropathies, painful neuropathies, ataxic
glycoprotein, ganglioside M , sulfatide moi- gait, bilateral foot drop
1
eties on peripheral nerve sheaths
Autoantibody activity to IgG Cryoglobulinemia (type II) Purpura, arthralgia, renal failure, sensorimotor
neuropathies
Autoantibody activity to red blood cell Cold agglutinins Hemolytic anemia, Raynaud phenomenon, acrocyanosis,
antigens livedo reticularis
Tissue deposition as amorphous aggregates Organ dysfunction Skin: bullous skin disease, papules, Schnitzler syndrome
Gastrointestinal: diarrhea, malabsorption, bleeding
Kidney: proteinuria, renal failure (light-chain component)
Tissue deposition as amyloid fibrils (light- Organ dysfunction Fatigue, weight loss, edema, hepatomegaly, macroglossia,
chain component most commonly) organ dysfunction of involved organs (heart, kidney, liver,
peripheral sensory and autonomic nerves)
Ig, immunoglobulin.
to inappropriately low erythropoietin production, which is the major viscosity is greater than 4.0 centipoises (cp), but there is individual vari-
reason for anemia in these patients. Renal synthesis of erythropoie- ability, with some patients showing no evidence of hyperviscosity even
67
tin is inversely correlated with plasma viscosity. Clinical manifestations at 10 cp. The most common symptoms are oronasal mucosal bleeding,
64
are related to circulatory disturbances that can be best appreciated by visual disturbances because of retinal bleeding, and dizziness that rarely
ophthalmoscopy, which shows distended and tortuous retinal veins, may lead to stupor or coma. Heart failure can be aggravated, particu-
hemorrhages, and papilledema (Fig. 109–3). Symptoms usually occur larly in the elderly, owing to increased blood viscosity, expanded plasma
68
when the monoclonal IgM concentration exceeds 50 g/L or when serum volume, and anemia. Inappropriate red cell transfusion can exacerbate
hyperviscosity and may precipitate cardiac failure.
Cryoglobulinemia
The monoclonal IgM can behave as a cryoglobulin in up to 20 percent
of patients, and is usually type I and asymptomatic in most cases. 16,64,70
Cryoprecipitation is mainly dependent on the concentration of mono-
clonal IgM; for this reason plasmapheresis or plasma exchange are com-
monly effective in this condition. Symptoms result from impaired blood
flow in small vessels and include Raynaud phenomenon, acrocyanosis,
and necrosis of the regions most exposed to cold, such as the tip of the
nose, ears, fingers, and toes (Fig. 109–4), malleolar ulcers, purpura, and
cold urticaria. Renal manifestations are infrequent. Mixed cryoglobu-
lins (type II) consisting of IgM–IgG complexes may be associated with
hepatitis C infections. 70
Autoantibody Activity
Monoclonal IgM may exert its pathogenic effects through specific rec-
ognition of autologous antigens, the most notable being nerve constitu-
ents, immunoglobulin determinants, and red blood cell antigens.
Immunoglobulin M–Related Neuropathy
IgM-related peripheral neuropathy is common in WM patients, with
estimated prevalence rates of 5 to 40 percent. 71–73 Approximately 8 per-
cent of idiopathic neuropathies are associated with a monoclonal gam-
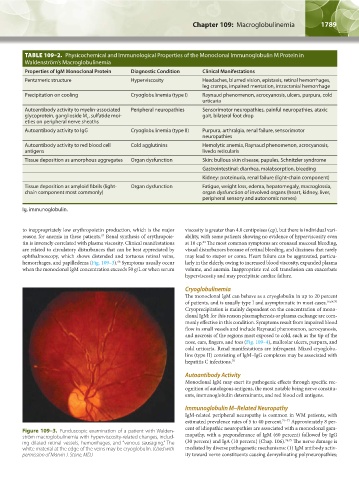
Figure 109–3. Funduscopic examination of a patient with Walden-
ström macroglobulinemia with hyperviscosity-related changes, includ- mopathy, with a preponderance of IgM (60 percent) followed by IgG
ing dilated retinal vessels, hemorrhages, and “venous sausaging.” The (30 percent) and IgA (10 percent) (Chap. 106). 74,75 The nerve damage is
white material at the edge of the veins may be cryoglobulin. (Used with mediated by diverse pathogenetic mechanisms: (1) IgM antibody activ-
permission of Marvin J. Stone, MD.) ity toward nerve constituents causing demyelinating polyneuropathies;
Kaushansky_chapter 109_p1785-1802.indd 1789 9/21/15 12:30 PM