Page 1966 - Williams Hematology ( PDFDrive )
P. 1966
1940 Part XII: Hemostasis and Thrombosis Chapter 113: Molecular Biology and Biochemistry of the Coagulation Factors 1941
NET DNA
Immunothrombosis
Fibrin
VWF
NET induction
Endothelial cell Neutrophil Monocyte
activation recruitment activation FXIIa
TF
Bacterium
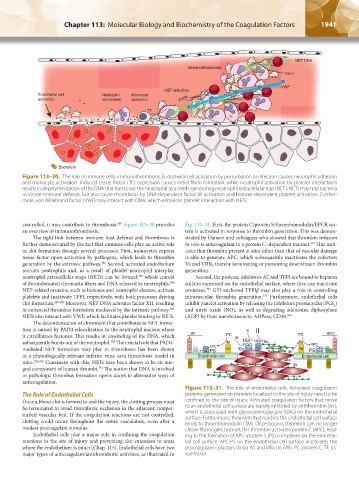
Figure 113–30. The role of immune cells: immunothrombosis. Endothelial cell activation by perturbation or infection causes neutrophil adhesion
and monocyte activation. Induced tissue factor (TF) expression causes initial fibrin formation, while neutrophil activation by platelet interactions
results in depolymerization of the DNA that bursts out the neutrophil as a mesh-generating neutrophil extracellular trap (NET). NETs may trap bacteria
as innate immune defense, but also cause thrombosis by DNA-dependent factor XII activation and histone-dependent platelet activation. Further-
more, von Willebrand factor (VWF) may interact with DNA, which enhances platelet interaction with NETs.
controlled, it may contribute to thrombosis. Figure 113–30 provides Fig. 113–31. First, the protein C/protein S/thrombomodulin/EPCR sys-
385
an overview of immunothrombosis. tem is activated in response to thrombin generation. This was demon-
The tight link between immune host defense and thrombosis is strated by Hanson and colleagues who showed that thrombin infusion
further demonstrated by the fact that immune cells play an active role in vivo is anticoagulant in a protein C–dependent manner. This indi-
392
in clot formation through several processes. First, monocytes express cates that thrombin present at sites other than that of vascular damage
tissue factor upon activation by pathogens, which leads to thrombin is able to generate APC, which subsequently inactivates the cofactors
generation by the extrinsic pathway. Second, activated endothelium Va and VIIIa, thereby terminating or preventing downstream thrombin
386
recruits neutrophils and, as a result of platelet-neutrophil interplay, generation.
neutrophil extracellular traps (NETs) can be formed, which consist Second, the protease inhibitors AT and TFPI are bound to heparan
387
of decondensated chromatin fibers and DNA released by neutrophils. sulfates expressed on the endothelial surface, where they can inactivate
388
NET-related proteins, such as histones and neutrophil elastase, activate proteases. GPI-anchored TFPIβ may also play a role in controlling
393
platelets and inactivate TFPI, respectively, with both processes driving intravascular thrombin generation. Furthermore, endothelial cells
332
clot formation. 338,389 Moreover, NET DNA activates factor XII, resulting inhibit platelet activation by releasing the inhibitors prostacyclin (PGI )
2
in enhanced thrombus formation mediated by the intrinsic pathway. and nitric oxide (NO), as well as degrading adenosine diphosphate
385
NETs also interact with VWF, which facilitates platelet binding to NETs. (ADP) by their membrane ecto-ADPase, CD39. 394
The decondensation of chromatin that contributes to NET forma-
tion is caused by PAD4 relocalization to the neutrophil nucleus where X II
it citrullinates histones. This results in unwinding of the DNA, which AT PC lX PC ATIII
subsequently bursts out of the neutrophil. The crucial role that PAD4- G lla lXa Xa lla lla APC G
388
lla
APC
mediated NET formation may play in thrombosis has been shown G A IV Va PS TM Xla VIIIa Va lla lla TM PS VIIIa iVIII A G
in a physiologically relevant inferior vena cava thrombosis model in Endothelial cell Activated platelet lla Endothelial cell
mice. 385,390 Consistent with this, NETs have been shown to be an inte- TF TF lla lla lla TF TF
gral component of human thrombi. The notion that DNA is involved lla lla
391
in pathologic thrombus formation opens doors to alternative ways of lla
anticoagulation.
Figure 113–31. The role of endothelial cells. Activated coagulation
The Role of Endothelial Cells proteins generated on platelets localized to the site of injury need to be
Once a blood clot is formed to seal the injury, the clotting process must confined to the site of injury. Activated coagulation factors that move
be terminated to avoid thrombotic occlusion in the adjacent, nonper- to an endothelial cell surface are rapidly inhibited by antithrombin (AT),
turbed vascular bed. If the coagulation reactions are not controlled, which is associated with glycosaminoglycans (GAG) on the endothelial
clotting could occur throughout the entire vasculature, even after a surface. Furthermore, thrombin that reaches the endothelial cell surface
binds to thrombomodulin (TM). Once bound, thrombin can no longer
modest procoagulant stimulus. cleave fibrinogen. Instead, this thrombin activates protein C (APC), lead-
Endothelial cells play a major role in confining the coagulation ing to the formation of APC–protein S (PS) complexes on the endothe-
reactions to the site of injury and preventing clot extension to areas lial cell surface. APC-PS on the endothelial cell surface inactivates the
where the endothelium is intact (Chap. 115). Endothelial cells have two procoagulant cofactors Va (to IV) and VIIIa (to iVIII). PC, protein C; TF, tis-
major types of anticoagulant/antithrombotic activities, as illustrated in sue factor.
Kaushansky_chapter 113_p1915-1948.indd 1941 9/21/15 2:41 PM