Page 878 - Williams Hematology ( PDFDrive )
P. 878
852 Part VI: The Erythrocyte Chapter 55: Alloimmune Hemolytic Disease of the Fetus and Newborn 853
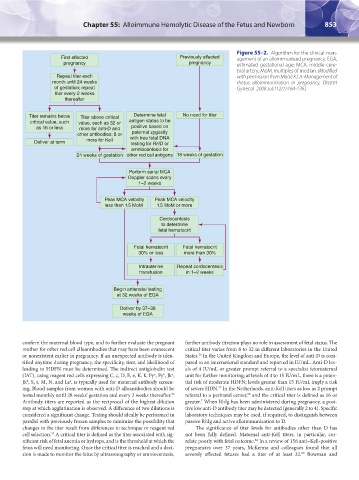
Figure 55–2. Algorithm for the clinical man-
First affected Previously affected agement of an alloimmunized pregnancy. EGA,
pregnancy pregnancy estimated gestational age; MCA, middle cere-
bral artery; MoM, multiples of median. (Modified
Repeat titer each with permission from Moise KJ Jr: Management of
month until 24 weeks rhesus alloimmunization in pregnancy. Obstet
of gestation; repeat Gynecol 2008 Jul;112(1):164-176.)
titer every 2 weeks
thereafter
Titer remains below Titer above critical Determine fetal No need for titer
critical value, such value, such as 32 or antigen status to be
as 16 or less more for anti-D and positive based on
paternal zygosity
other antibodies; 8 or with free fetal DNA
Deliver at term more for Kell testing for RHD or
amniocentesis for
24 weeks of gestation other red cell antigens 18 weeks of gestation
Perform serial MCA
Doppler scans every
1–2 weeks
Peak MCA velocity Peak MCA velocity
less than 1.5 MoM 1.5 MoM or more
Cordocentesis
to determine
fetal hematocrit
Fetal hematocrit Fetal hematocrit
30% or less more than 30%
Intrauterine Repeat cordocentesis
transfusion in 1–2 weeks
Begin antenatal testing
at 32 weeks of EGA
Deliver by 37–38
weeks of EGA
confirm the maternal blood type, and to further evaluate the pregnant further antibody titration plays no role in assessment of fetal status. The
mother for other red cell alloantibodies that may have been evanescent critical titer varies from 8 to 32 in different laboratories in the United
or nonexistent earlier in pregnancy. If an unexpected antibody is iden- States. In the United Kingdom and Europe, the level of anti-D is com-
76
tified anytime during pregnancy, the specificity, titer, and likelihood of pared to an international standard and reported in IU/mL. Anti-D lev-
leading to HDFN must be determined. The indirect antiglobulin test els of 4 IU/mL or greater prompt referral to a specialist fetomaternal
(IAT), using reagent red cells expressing C, c, D, E, e, K, k, Fy , Fy , Jk , unit for further monitoring; at levels of 4 to 15 IU/mL, there is a poten-
b
a
a
Jk , S, s, M, N, and Le , is typically used for maternal antibody screen- tial risk of moderate HDFN; levels greater than 15 IU/mL imply a risk
b
a
ing, Blood samples from women with anti-D alloantibodies should be of severe HDN. In the Netherlands, anti-Kell titers as low as 2 prompt
77
tested monthly until 28 weeks’ gestation and every 2 weeks thereafter. referral to a perinatal center, and the critical titer is defined as 16 or
59
76
Antibody titers are reported as the reciprocal of the highest dilution greater. When RhIg has been administered during pregnancy, a posi-
7
step at which agglutination is observed. A difference of two dilutions is tive low anti-D antibody titer may be detected (generally 2 to 4). Specific
considered a significant change. Testing should ideally be performed in laboratory techniques may be used, if required, to distinguish between
parallel with previously frozen samples to minimize the possibility that passive RhIg and active alloimmunization to D.
changes in the titer result from differences in technique or reagent red The significance of titer levels for antibodies other than D has
cell selection. A critical titer is defined as the titer associated with sig- not been fully defined. Maternal anti-Kell titers, in particular, cor-
57
nificant risk of fetal anemia or hydrops, and is the threshold at which the relate poorly with fetal outcome. In a review of 156 anti–Kell-positive
62
fetus will need monitoring. Once the critical titer is reached and a deci- pregnancies over 37 years, McKenna and colleagues found that all
sion is made to monitor the fetus by ultrasonography or amniocentesis, severely affected fetuses had a titer of at least 32. Bowman and
60
Kaushansky_chapter 55_p0847-0862.indd 853 9/18/15 11:52 PM