Page 994 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 994
CHaPter 71 Type 1 Diabetes 959
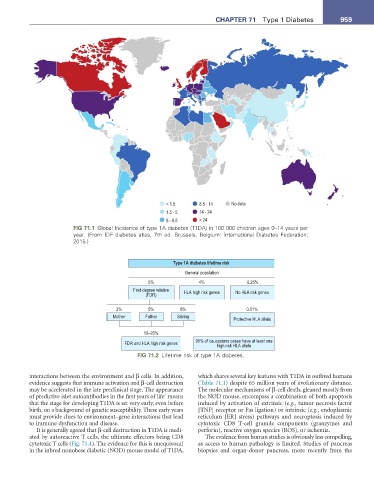
< 1.5 8.5 - 14 No data
1.5 - 5 14 - 24
5 - 8.5 > 24
FIG 71.1 Global Incidence of type 1A diabetes (T1DA) in 100 000 children ages 0–14 years per
year. (From IDF diabetes atlas, 7th ed. Brussels, Belgium: International Diabetes Federation;
2015.)
Type 1A diabetes lifetime risk
General population
5% 4% 0.25%
First-degree relative HLA high risk genes No HLA risk genes
(FDR)
3% 5% 8% 0.01%
Mother Father Sibling
Protective HLA allele
10–20%
FDR and HLA high risk genes 95% of caucasians cases have at least one
high risk HLA allele
FIG 71.2 Lifetime risk of type 1A diabetes.
interactions between the environment and β cells. In addition, which shares several key features with T1DA in outbred humans
evidence suggests that immune activation and β-cell destruction (Table 71.1) despite 65 million years of evolutionary distance.
may be accelerated in the late preclinical stage. The appearance The molecular mechanisms of β-cell death, gleaned mostly from
5
of predictive islet autoantibodies in the first years of life means the NOD mouse, encompass a combination of both apoptosis
that the stage for developing T1DA is set very early, even before induced by activation of extrinsic (e.g., tumor necrosis factor
birth, on a background of genetic susceptibility. These early years [TNF] receptor or Fas ligation) or intrinsic (e.g., endoplasmic
must provide clues to environment–gene interactions that lead reticulum [ER] stress) pathways and necroptosis induced by
to immune dysfunction and disease. cytotoxic CD8 T-cell granule components (granzymes and
It is generally agreed that β-cell destruction in T1DA is medi- perforin), reactive oxygen species (ROS), or ischemia.
ated by autoreactive T cells, the ultimate effectors being CD8 The evidence from human studies is obviously less compelling,
cytotoxic T cells (Fig. 71.4). The evidence for this is unequivocal as access to human pathology is limited. Studies of pancreas
in the inbred nonobese diabetic (NOD) mouse model of T1DA, biopsies and organ-donor pancreas, more recently from the