Page 995 - Clinical Immunology_ Principles and Practice ( PDFDrive )
P. 995
960 Part seven Organ-Specific Inflammatory Disease
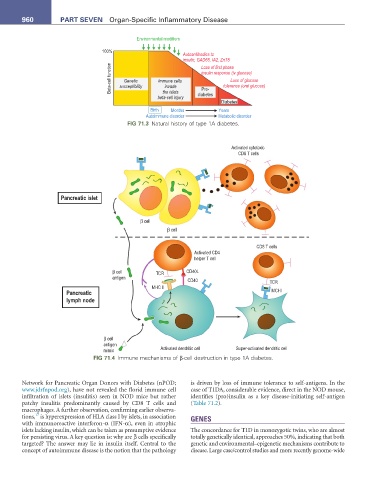
Environmental modifiers
100%
Autoantibodies to
insulin, GAD65, IA2, ZnT8
Beta-cell function susceptibility Immune cells insulin response (iv glucose)
Loss of first phase
Loss of glucose
Genetic
tolerance (oral glucose)
invade
Pre-
the islets
beta-cell injury diabetes
Diabetes
Birth Months Years
Autoimmune disorder Metabolic disorder
FIG 71.3 Natural history of type 1A diabetes.
Activated cytotoxic
CD8 T cells
Pancreatic islet
β cell
β cell
CD8 T cells
Activated CD4
helper T cell
β cell TCR CD40L
antigen
CD40 TCR
MHC II
Pancreatic MCHI
lymph node
β cell
antigen
mimic Activated dendritic cell Super-activated dendritic cell
FIG 71.4 Immune mechanisms of β-cell destruction in type 1A diabetes.
Network for Pancreatic Organ Donors with Diabetes (nPOD; is driven by loss of immune tolerance to self-antigens. In the
www.jdrfnpod.org), have not revealed the florid immune cell case of T1DA, considerable evidence, direct in the NOD mouse,
infiltration of islets (insulitis) seen in NOD mice but rather identifies (pro)insulin as a key disease-initiating self-antigen
patchy insulitis predominantly caused by CD8 T cells and (Table 71.2).
macrophages. A further observation, confirming earlier observa-
17
tions, is hyperexpression of HLA class I by islets, in association GENES
with immunoreactive interferon-α (IFN-α), even in atrophic
islets lacking insulin, which can be taken as presumptive evidence The concordance for T1D in monozygotic twins, who are almost
for persisting virus. A key question is: why are β cells specifically totally genetically identical, approaches 50%, indicating that both
targeted? The answer may lie in insulin itself. Central to the genetic and environmental–epigenetic mechanisms contribute to
concept of autoimmune disease is the notion that the pathology disease. Large case/control studies and more recently genome-wide