Page 1501 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1501
1040 PART 9: Gastrointestinal Disorders
not directly involved, hypotension may combine with pseudocoarctation present in advanced mesenteric ischemia with sepsis or perforation.
to provoke ischemia or occlusion via a dissection flap), aortic trauma, Arterial blood gases frequently are normal initially, but in the later
mesenteric aneurysm rupture, arteritis, fibromuscular dysplasia (FMD), stages, metabolic acidosis and acute hypoxemia may supervene. Lactic
and extrinsic mechanical vascular obstruction. Acute intestinal ischemia acidosis is often a late finding. Prerenal azotemia is a grave indicator,
also may arise as a result of extrinsic mechanical compression of the signaling hypovolemia, sepsis, nephrotoxic effect, or disseminated intra-
arterial inflow or venous outflow. As low-pressure conduits, veins are vascular coagulation (DIC). The erythrocyte sedimentation rate (ESR)
most susceptible to extrinsic compression; intramural venous plexi may and later C-reactive protein (CRP) level may rise. Potential alternative
be obstructed due to wall distention, whereas mesenteric veins may be serum markers, such as creatinine kinase (CK) BB isoenzyme, lactate
compressed by tumor, adhesion, volvulus, hernia, or intussusception. dehydrogenase, intestinal isoenzyme of alkaline phosphatase, diamine
oxidase, hexosaminidase, and aspartate transferase, have not proved suf-
DIAGNOSIS OF ACUTE MESENTERIC ISCHEMIA ficiently sensitive or specific. The most encouraging markers are serum
inorganic phosphate, α-glutathione-S-transferase, and d-lactate.
29
28
27
The single most important factor is clinical suspicion followed by inves- A recent review of plasma biomarkers in acute mesenteric ischemia has
tigation. A delay in diagnosis may be lethal. No single blood marker reviewed those markers noted above including intestinal fatty acid bind-
20
has proved to be an adequate screening test. Lactic acidosis has poor ing globulin (I-FABP) and concluded that none are definitive. Further
sensitivity in detecting bowel ischemia. Arterial phase CT angiogram prospective clinical studies were suggested on those patients presenting
with oral contrast allows imaging of the arterial tree as well as the bowel with acute abdominal pain to determine if the proposed markers can be
wall. Thickening of the bowel wall and intestinal pneumatosis can all be shown to aid in the early diagnosis of mesenteric ischemia. 65
imaged simultaneously and rapidly (CT scan can be performed plain,
then with arterial phase, and venous phases to obtain maximal informa- ■ PLAIN ABDOMINAL RADIOGRAM
tion). Conventional mesenteric angiography offers the ability to inter-
vene with angioplasty and remains an important tool for diagnosis and Plain abdominal radiographs may reveal supporting information such as
therapy. In addition, a selective catheter placed in the SMA can allow heavy calcification of the abdominal vasculature, although this is neither
for arterial drug infusion. Even with high-quality imaging studies, lapa- sensitive nor specific. In a retrospective series of 23 patients with acute
rotomy may be required for definitive diagnosis. A suggested algorithm mesenteric ischemia, 26% had normal plain films. Nonspecific signs of
for the initial approach to a patient with suspected acute mesenteric ischemia, such as intestinal dilation or gasless abdomen, may be present,
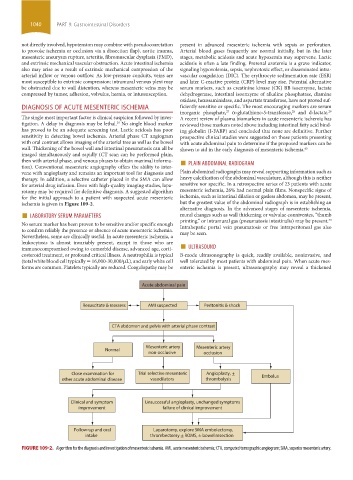
ischemia is given in Figure 109-2. but the greatest value of the abdominal radiograph is in establishing an
■ LABORATORY SERUM PARAMETERS mural changes such as wall thickening or valvulae conniventes, “thumb
alternative diagnosis. In the advanced stages of mesenteric ischemia,
30
No serum marker has been proven to be sensitive and/or specific enough printing,” or intramural gas (pneumatosis intestinalis) may be present.
Intrahepatic portal vein pneumatosis or free intraperitoneal gas also
to confirm reliably the presence or absence of acute mesenteric ischemia. may be seen.
Nevertheless, some are clinically useful. In acute mesenteric ischemia, a
immunocompromised owing to comorbid disease, advanced age, corti- ■ ULTRASOUND
leukocytosis is almost invariably present, except in those who are
costeroid treatment, or profound critical illness. A neutrophilia is typical B-mode ultrasonography is quick, readily available, noninvasive, and
(total white blood cell typically = 16,000-30,000/µL), and early white cell well tolerated by most patients with abdominal pain. When acute mes-
forms are common. Platelets typically are reduced. Coagulopathy may be enteric ischemia is present, ultrasonography may reveal a thickened
Acute abdominal pain
Resuscitate & reassess AMI suspected Peritonitis & shock
CTA abdomen and pelvis with arterial phase contrast
Mesenteric artery Mesenteric artery
Normal
non-occlusive occlusion
Close examination for Trial selective mesenteric Angioplasty,
other acute abdominal disease vasodilators thrombolysis Embolus
Clinical and symptom Unsuccessful angioplasty, unchanged symptoms
improvement failure of clinical improvement
Follow-up and oral Laparotomy, explore SMA embolectomy,
intake thrombectomy ROMS, bowel resection
FIGURE 109-2. Algorithm for the diagnosis and investigation of mesenteric ischemia. AMI, acute mesenteric ischemia; CTA, computed tomographic angiogram; SMA, superior mesenteric artery.
section09.indd 1040 1/14/2015 9:27:27 AM