Page 1650 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1650
CHAPTER 121: Pelvic Ring Injuries and Extremity Trauma 1169
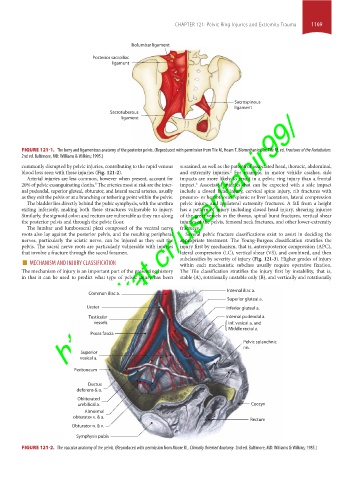
Iliolumbar ligament
Posterior sacroiliac
ligament
Sacrospinous
ligament
https://kat.cr/user/tahir99/
Sacrotuberous
ligament
FIGURE 121-1. The bony and ligamentous anatomy of the posterior pelvis. (Reproduced with permission from Tile M, Hearn T. Biomechanics. In: Tile M, ed. Fractures of the Acetabulum.
2nd ed. Baltimore, MD: Williams & Wilkins; 1995.)
commonly disrupted by pelvic injuries, contributing to the rapid venous sustained, as well as the pattern of associated head, thoracic, abdominal,
blood loss seen with these injuries (Fig. 121-2). and extremity injuries. For example, in motor vehicle crashes, side
2
Arterial injuries are less common, however when present, account for impacts are more likely to result in a pelvic ring injury than a frontal
20% of pelvic exsanguinating deaths. The arteries most at risk are the inter- impact. Associated injuries that can be expected with a side impact
5
6
nal pudendal, superior gluteal, obturator, and lateral sacral arteries, usually include a closed head injury, cervical spine injury, rib fractures with
as they exit the pelvis or at a branching or tethering point within the pelvis. pneumo- or hemothorax, splenic or liver laceration, lateral compression
The bladder lies directly behind the pubic symphysis, with the urethra pelvic injury, and ipsilateral extremity fractures. A fall from a height
exiting inferiorly, making both these structures vulnerable to injury. has a pattern of injury including closed head injury, shearing injuries
Similarly, the sigmoid colon and rectum are vulnerable as they run along of the great vessels in the thorax, spinal burst fractures, vertical shear
the posterior pelvis and through the pelvic floor. injuries of the pelvis, femoral neck fractures, and other lower-extremity
The lumbar and lumbosacral plexi composed of the ventral nerve fractures.
roots also lay against the posterior pelvis, and the resulting peripheral Several pelvic fracture classifications exist to assist in deciding the
nerves, particularly the sciatic nerve, can be injured as they exit the appropriate treatment. The Young-Burgess classification stratifies the
pelvis. The sacral nerve roots are particularly vulnerable with injuries injury first by mechanism, that is, anteroposterior compression (APC),
that involve a fracture through the sacral foramen. lateral compression (LC), vertical shear (VS), and combined, and then
■ MECHANISM AND INJURY CLASSIFICATION subclassifies by severity of injury (Fig. 121-3). Higher grades of injury
within each mechanistic subclass usually require operative fixation.
The mechanism of injury is an important part of the presenting history The Tile classification stratifies the injury first by instability, that is,
in that it can be used to predict what type of pelvic injury has been stable (A), rotationally unstable only (B), and vertically and rotationally
Internal iliac a.
Common iliac a.
Superior gluteal a.
Ureter Inferior gluteal a.
Testicular Internal pudendal a.
vessels Inf. vesical a. and
Middle rectal a.
Psoas fascia
Pelvic splanchnic
nn.
Superior
vesical a.
Peritoneum
Ductus
deferens & a.
Obliterated
umbilical a. Coccyx
Abnormal
obturator v. & a.
Rectum
Obturator n. & v.
Symphysis pubis
FIGURE 121-2. The vascular anatomy of the pelvis. (Reproduced with permission from Moore KL. Clinically Oriented Anatomy. 2nd ed. Baltimore, MD: Williams & Wilkins; 1985.)
section10.indd 1169 1/20/2015 9:21:17 AM