Page 1787 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1787
1256 PART 11: Special Problems in Critical Care
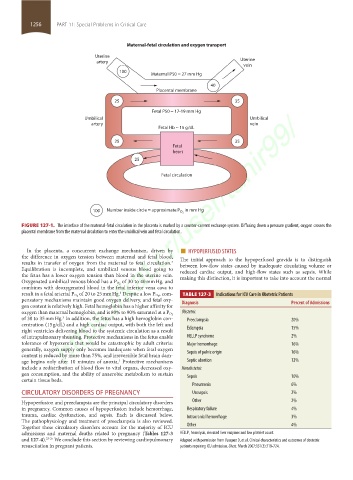
Maternal-fetal circulation and oxygen transport
Uterine
artery Uterine
vein
100 Maternal P50 = 27 mm Hg
40
Placental membrane
25 35
https://kat.cr/user/tahir99/
Fetal P50 = 17-19 mm Hg
Umbilical Umbilical
artery vein
Fetal Hb ~ 15 g/dL
25 35
Fetal
heart
25
Fetal circulation
100 Number inside circle = approximate P O 2 in mm Hg
FIGURE 127-1. The interface of the maternal-fetal circulation in the placenta is marked by a counter-current exchange system. Diffusing down a pressure gradient, oxygen crosses the
placental membrane from the maternal circulation to enter the umbilical vein and fetal circulation.
In the placenta, a concurrent exchange mechanism, driven by ■ HYPOPERFUSED STATES
the difference in oxygen tension between maternal and fetal blood, The initial approach to the hypoperfused gravida is to distinguish
results in transfer of oxygen from the maternal to fetal circulation. between low-flow states caused by inadequate circulating volume or
3
Equilibration is incomplete, and umbilical venous blood going to reduced cardiac output, and high-flow states such as sepsis. While
the fetus has a lower oxygen tension than blood in the uterine vein. making this distinction, it is important to take into account the normal
of 30 to 40 mm Hg, and
Oxygenated umbilical venous blood has a P O 2
combines with deoxygenated blood in the fetal inferior vena cava to
3 , com-
result in a fetal arterial P O 2 of 20 to 25 mm Hg. Despite a low P O 2 TABLE 127-3 Indications for ICU Care in Obstetric Patients
pensatory mechanisms maintain good oxygen delivery, and fetal oxy- Diagnosis Percent of Admissions
gen content is relatively high. Fetal hemoglobin has a higher affinity for
Obstetric
oxygen than maternal hemoglobin, and is 80% to 90% saturated at a P O 2
of 30 to 35 mm Hg. In addition, the fetus has a high hemoglobin con- Preeclampsia 20%
3
centration (15 g/dL) and a high cardiac output, with both the left and
right ventricles delivering blood to the systemic circulation as a result Eclampsia 15%
of intrapulmonary shunting. Protective mechanisms in the fetus enable HELLP syndrome 2%
tolerance of hypoxemia that would be catastrophic by adult criteria: Major hemorrhage 16%
generally, oxygen supply only becomes inadequate when fetal oxygen Sepsis of pelvic origin 16%
content is reduced by more than 75%, and irreversible fetal brain dam-
age begins only after 10 minutes of anoxia. Protective mechanisms Septic abortion 12%
3
include a redistribution of blood flow to vital organs, decreased oxy- Nonobstetric
gen consumption, and the ability of anaerobic metabolism to sustain Sepsis 10%
certain tissue beds.
Pneumonia 6%
CIRCULATORY DISORDERS OF PREGNANCY Urosepsis 2%
Hypoperfusion and preeclampsia are the principal circulatory disorders Other 2%
in pregnancy. Common causes of hypoperfusion include hemorrhage, Respiratory failure 4%
trauma, cardiac dysfunction, and sepsis. Each is discussed below. Intracranial hemorrhage 3%
The pathophysiology and treatment of preeclampsia is also reviewed.
Together these circulatory disorders account for the majority of ICU Other 4%
admissions and maternal deaths related to pregnancy (Tables 127-3 HELLP, hemolysis, elevated liver enzymes and low platelet count.
and 127-4). 23-25 We conclude this section by reviewing cardiopulmonary Adapted with permission from Vasquez D, et al. Clinical characteristics and outcomes of obstetric
resuscitation in pregnant patients. patients requiring ICU admission. Chest. March 2007;131(3):718-724.
section11.indd 1256 1/19/2015 10:52:20 AM