Page 1788 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1788
CHAPTER 127: Critical Illness in Pregnancy 1257
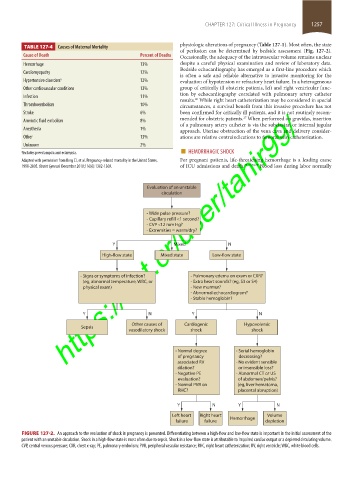
physiologic alterations of pregnancy (Table 127-1). Most often, the state
TABLE 127-4 Causes of Maternal Mortality
of perfusion can be determined by bedside assessment (Fig. 127-2).
Cause of Death Percent of Deaths Occasionally, the adequacy of the intravascular volume remains unclear
Hemorrhage 13% despite a careful physical examination and review of laboratory data.
Bedside echocardiography has emerged as a first-line procedure which
Cardiomyopathy 12%
is often a safe and reliable alternative to invasive monitoring for the
Hypertensive disorders a 12% evaluation of hypotension or refractory heart failure. In a heterogeneous
Other cardiovascular conditions 12% group of critically ill obstetric patients, left and right ventricular func-
tion by echocardiography correlated with pulmonary artery catheter
Infection 11%
results. While right heart catheterization may be considered in special
26
Thromboembolism 10% circumstances, a survival benefit from this invasive procedure has not
https://kat.cr/user/tahir99/
Stroke 6% been confirmed for critically ill patients, and it is not routinely recom-
mended for obstetric patients. When performed on gravidas, insertion
27
Amniotic fluid embolism 8%
of a pulmonary artery catheter is via the subclavian or internal jugular
Anesthesia 1% approach. Uterine obstruction of the vena cava and delivery consider-
Other 13% ations are relative contraindications to femoral vein catheterization.
Unknown 2%
a Includes preeclampsia and eclampsia. ■ HEMORRHAGIC SHOCK
Adapted with permission from Berg CJ, et al. Pregnancy-related mortality in the United States, For pregnant patients, life-threatening hemorrhage is a leading cause
1998-2005. Obstet Gynecol. December 2010;116(6):1302-1309. of ICU admissions and death. 23,24,28,29 Blood loss during labor normally
Evaluation of an unstable
circulation
- Wide pulse pressure?
- Capillary refill <1 second?
- CVP <12 mm Hg?
- Extremities = warm/dry?
Y Mixed N
High-flow state Mixed state Low-flow state
- Signs or symptoms of infection? - Pulmonary edema on exam or CXR?
(eg, abnormal temperature, WBC, or - Extra heart sounds? (eg, S3 or S4)
physical exam) - New murmur?
- Abnormal echocardiogram?
- Stable hemoglobin?
Y N Y N
Other causes of Cardiogenic Hypovolemic
Sepsis
vasodilatory shock shock shock
- Normal degree - Serial hemoglobin
of pregnancy decreasing?
associated RV - No evident sensible
dilation? or insensible loss?
- Negative PE - Abnormal CT or US
evaluation? of abdomen/pelvis?
- Normal PVR on (eg, liver hematoma,
RHC? placental abruption)
Y N Y N
Left heart Right heart Hemorrhage Volume
failure failure depletion
FIGURE 127-2. An approach to the evaluation of shock in pregnancy is presented. Differentiating between a high-flow and low-flow state is important in the initial assessment of the
patient with an unstable circulation. Shock in a high-flow state is most often due to sepsis. Shock in a low-flow state is attributable to impaired cardiac output or a depleted circulating volume.
CVP, central venous pressure; CXR, chest x-ray; PE, pulmonary embolism; PVR, peripheral vascular resistance; RHC, right heart catheterization; RV, right ventricle; WBC, white blood cells.
section11.indd 1257 1/19/2015 10:52:20 AM