Page 1156 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 1156
CHAPTER 86: Intracranial Pressure: Monitoring and Management 795
A B tissue, whether CSF outlets are obstructed, and whether the volume of
the space-occupying lesion causing tissue shift is large enough to over-
come compensatory mechanisms. Regional mass effect can cause brain
damage through local effects on brain perfusion and exertion of direct
mechanical injury to tissue in the absence of globally elevated ICP. Brain
tissue displacement can cause depressed consciousness through distor-
tion of key anatomical structures responsible for arousal and attention
(diencephalon and brainstem) in the absence of global increases in ICP.
Similarly, while reduced consciousness can be the result of elevated ICP
secondary to tissue displacement and herniation, it may be seen as a late
sign following earlier symptoms relevant to the direct compression of
underlying structures. For example, autonomic changes can occur early
with evolving BTD, and their recognition can serve as a warning sign
of impending herniation. The clinical consequences of BTD depend
27
on the etiology, location, size of the lesion, and duration of the pro-
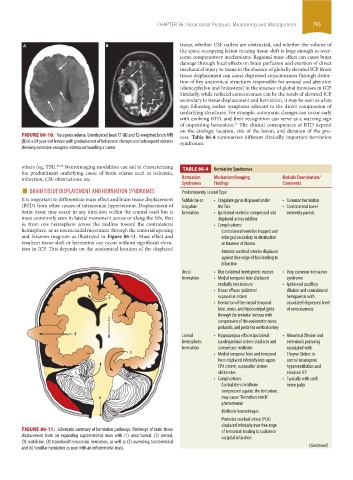
FIGURE 86-10. Vasogenic edema. Unenhanced head CT (A) and T2-weighted brain MRI cess. Table 86-4 summarizes different clinically important herniation
(B) in a 64 year-old female with gradual onset of behavioral changes and subsequent seizures syndromes.
showing extensive vasogenic edema surrounding a tumor.
others (eg, TBI). 25,26 Neuroimaging modalities can aid in characterizing TABLE 86-4 Herniation Syndromes
the predominant underlying cause of brain edema such as ischemia,
infarction, CSF obstructions, etc. Herniation Mechanism/Imaging Bedside Examination/
■ BRAIN TISSUE DISPLACEMENT AND HERNIATION SYNDROMES Predominantly Lateral Type
Comments
Findings
Syndromes
It is important to differentiate mass effect and brain tissue displacement Subfalcine or • Cingulate gyrus displaced under • Common herniation
(BTD) from other causes of intracranial hypertension. Displacement of cingulate the falx • Contralateral lower
brain tissue may occur in any direction within the cranial vault but is herniation • Ipsilateral ventricle compressed and extremity paresis
most commonly seen in lateral movement across or along the falx, that displaced across midline
is, from one hemisphere across the midline toward the contralateral • Complications:
hemisphere, or as rostrocaudal movement through the tentorial opening Contralateral ventricle trapped and
and foramen magnum as illustrated in Figure 86-11. Mass effect and enlarged secondary to obstruction
resultant tissue shift or herniation can occur without significant eleva- at foramen of Monro
tion in ICP. This depends on the anatomical location of the displaced Anterior cerebral arteries displaced
against free edge of falx leading to
infarction
Uncal • Due to lateral hemispheric masses • Very common herniation
herniation • Medial temporal lobe displaced syndrome
medially into incisura • Ipsilateral pupillary
• Uncus effaces ipsilateral dilation and contralateral
3 suprasellar cistern hemiparesis with
• Herniation of the mesial temporal associated depressed level
lobe, uncus, and hippocampal gyrus of consciousness
through the tentorial incisura with
2 compression of the oculomotor nerve,
peduncle, and posterior cerebral artery
4 Lateral • Hippocampus effaces ipsilateral • Abnormal (flexion and
hemispheric quadrigeminal cistern displaces and extension) posturing
herniation compresses midbrain associated with
1 • Medial temporal lobe and temporal Cheyne-Stokes to
horn displaced inferiorly into upper central neurogenic
CPA cistern, suprasellar cistern hyperventilation and
5 obliterates elevated ICP
• Complications: • Typically with sixth
Contralateral midbrain nerve palsy
compressed against the tentorium,
6 may cause “Kernohan notch”
phenomenon
Midbrain hemorrhages
Posterior cerebral artery (PCA)
displaced inferiorly over free edge
FIGURE 86-11. Schematic summary of herniation pathways. Pathways of brain tissue of tentorium leading to ipsilateral
displacement from an expanding supratentorial mass with (1) uncal/lateral, (2) central, occipital infarction
(3) subfalcine, (4) transdural/transcranial herniation, as well as (5) ascending transtentorial
and (6) tonsillar herniation as seen with an infratentorial mass. (Continued)
section06.indd 795 1/23/2015 12:55:53 PM