Page 435 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 435
CHAPTER 37: Myocardial Ischemia 305
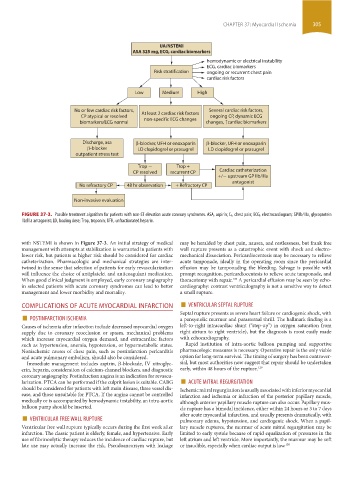
UA/NSTEMI
ASA 325 mg, ECG, cardiac biomarkers
hemodynamic or electrical instability
ECG, cardiac biomarkers
Risk stratification ongoing or recurrent chest pain
cardiac risk factors
Low Medium High
No or few cardiac risk factors, At least 2 cardiac risk factors Several cardiac risk factors,
CP atypical or resolved ongoing CP, dynamic ECG
biomarkers/ECG normal non-specific ECG changes changes, ↑cardiac biomarkers
Discharge, asa β-blocker, UFH or enoxaparin β-blocker, UFH or enoxaparin
β-blocker LD clopidogrel or prasugrel LD clopidogrel or prasugrel
outpatient stress test
Trop - Trop +
CP resolved recurrent CP Cardiac catheterization
+/- upstream GP IIb/IIIa
antagonist
No refractory CP 48 hr observation + Refractory CP
Non-invasive evaluation
FIGURE 37-3. Possible treatment algorithm for patients with non-ST elevation acute coronary syndromes. ASA, aspirin; C P, chest pain; ECG, electrocardiogram; GPIIb/IIIa, glycoprotein
IIb/IIIa antagonist; LD, loading dose; Trop, troponin; UFH, unfractionated heparin.
with NSTEMI is shown in Figure 37-3. An initial strategy of medical may be heralded by chest pain, nausea, and restlessness, but frank free
management with attempts at stabilization is warranted in patients with wall rupture presents as a catastrophic event with shock and electro-
lower risk, but patients at higher risk should be considered for cardiac mechanical dissociation. Pericardiocentesis may be necessary to relieve
catheterization. Pharmacologic and mechanical strategies are inter- acute tamponade, ideally in the operating room since the pericardial
twined in the sense that selection of patients for early revascularization effusion may be tamponading the bleeding. Salvage is possible with
will influence the choice of antiplatelet and anticoagulant medication. prompt recognition, pericardiocentesis to relieve acute tamponade, and
When good clinical judgment is employed, early coronary angiography thoracotomy with repair. A pericardial effusion may be seen by echo-
128
in selected patients with acute coronary syndromes can lead to better cardiography: contrast ventriculography is not a sensitive way to detect
management and lower morbidity and mortality. a small rupture.
COMPLICATIONS OF ACUTE MYOCARDIAL INFARCTION ■ VENTRICULAR SEPTAL RUPTURE
■ POSTINFARCTION ISCHEMIA Septal rupture presents as severe heart failure or cardiogenic shock, with
a pansystolic murmur and parasternal thrill. The hallmark finding is a
Causes of ischemia after infarction include decreased myocardial oxygen left-to-right intracardiac shunt (“step-up”) in oxygen saturation from
supply due to coronary reocclusion or spasm, mechanical problems right atrium to right ventricle), but the diagnosis is most easily made
which increase myocardial oxygen demand, and extracardiac factors with echocardiography.
such as hypertension, anemia, hypotension, or hypermetabolic states. Rapid institution of intra-aortic balloon pumping and supportive
Nonischemic causes of chest pain, such as postinfarction pericarditis pharmacologic measures is necessary. Operative repair is the only viable
and acute pulmonary embolism, should also be considered. option for long-term survival. The timing of surgery has been controver-
Immediate management includes aspirin, β-blockade, IV nitroglyc- sial, but most authorities now suggest that repair should be undertaken
erin, heparin, consideration of calcium-channel blockers, and diagnostic early, within 48 hours of the rupture. 129
coronary angiography. Postinfarction angina is an indication for revascu- ■
larization. PTCA can be performed if the culprit lesion is suitable. CABG ACUTE MITRAL REGURGITATION
should be considered for patients with left main disease, three vessel dis- Ischemic mitral regurgitation is usually associated with inferior myocardial
ease, and those unsuitable for PTCA. If the angina cannot be controlled infarction and ischemia or infarction of the posterior papillary muscle,
medically or is accompanied by hemodynamic instability, an intra-aortic although anterior papillary muscle rupture can also occur. Papillary mus-
balloon pump should be inserted. cle rupture has a bimodal incidence, either within 24 hours or 3 to 7 days
■ VENTRICULAR FREE WALL RUPTURE after acute myocardial infarction, and usually presents dramatically, with
pulmonary edema, hypotension, and cardiogenic shock. When a papil-
Ventricular free wall rupture typically occurs during the first week after lary muscle ruptures, the murmur of acute mitral regurgitation may be
infarction. The classic patient is elderly, female, and hypertensive. Early limited to early systole because of rapid equalization of pressures in the
use of fibrinoolytic therapy reduces the incidence of cardiac rupture, but left atrium and left ventricle. More importantly, the murmur may be soft
late use may actually increase the risk. Pseudoaneursym with leakage or inaudible, especially when cardiac output is low. 130
section03.indd 305 1/23/2015 2:07:22 PM