Page 621 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 621
CHAPTER 51: Ventilator-Induced Lung Injury 441
injury (ALI)/ARDS. Moreover, in established ARDS, tidal volume A Average Average
reduction associated with the application of PEEP attenuates these lung weight, lung weight,
phenomena. 59 ± 51 g 374 ± 236 g
Lower Higher
Shortly after the institution of invasive positive pressure ventilation,
the development of lung damage was observed in animals ventilated 24
22
for prolonged periods. The term “respirator lung” was coined to 5% ± 4% 21% ±10% Patients with acute lung
describe the functional and histologic features. In 1974, Webb and 20 injury without ARDS
26
18
Tierney graphically illustrated the deleterious effects of mechanical 16 Patients with ARDS
ventilation in rats using varying levels of peak airway pressure and 14
PEEP. Animals ventilated using low peak airway pressures (14 cm No. of patients 12
27
H O and no PEEP) had no pathologic or physiologic changes. In con- 10
2
trast, rats ventilated with peak pressures of 30 cm H O and no PEEP 8
2
had perivascular edema and alveolar edema. These findings were mag- 6
nified in rats ventilated with peak pressures of 45 cm H O. Alveolar 4
2
and perivascular edema developed, along with severe hypoxemia, 2
decreased dynamic compliance, and obvious gross anatomic changes 0
(Fig. 51-1). Interestingly, rats ventilated using 10 cm H O of PEEP and −5 to 0 0 to 5 5 to 10 10 to 15 15 to 20 20 to 25 25 to 30 30 to 35 35 to 40 40 to 45 45 to 50 50 to 55 55 to 60 60 to 65 65 to 70 70 to 75 75 to 80
2
peak pressures of 45 cm H O had no alveolar edema (see Fig. 51-1, −10 to −5
2
center). This latter finding led to the concept of a protective effect of Amount of potentially recruitable lung (% total lung weight)
PEEP, which will be discussed later.
Subsequent investigations have demonstrated that mechanical ven- B Lower percentage of potentially recruitable lung
tilation, even at modest airway pressures, is capable of producing 5 cm of water 45 cm of water
functional impairment of the lung with loss of integrity of the alveolar-
capillary barrier, surfactant dysfunction, and parenchymal damage that
mimics the histologic appearance of ARDS. These observations have
led investigators to speculate that mechanical ventilation itself could be
contributing to the lung injury, morbidity, and mortality in patients with
acute respiratory failure.
Numerous human studies demonstrate that mechanical ventilation
with large tidal volumes is capable of inciting lung inflammation and
may lead to the development of ALI/ARDS. 28,29 Patients with underlying C Higher percentage of potentially recruitable lung
lung disease are particularly prone to the development of macroscopic 5 cm of water 45 cm of water
barotrauma. Asthma, chronic obstructive pulmonary disease (COPD),
and pneumonia have all been identified as risk factors. 12
■ HIGH AIRWAY PRESSURES/LARGE TIDAL VOLUMES AND LUNG INJURY
• Transpulmonary pressure—the pressure difference between the alve-
oli and the pleural space is the effective alveolar distending pressure
and is the pressure most closely related to the development of VILI.
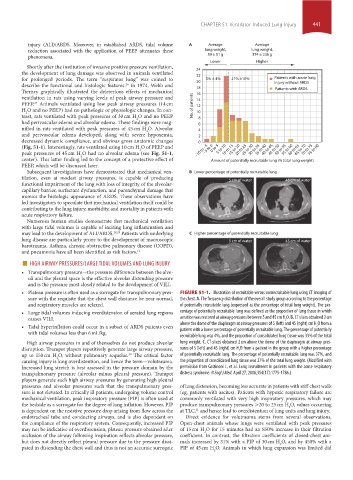
• Plateau pressure is often used as a surrogate for transpulmonary pres- FIGURE 51-1. Illustration of recruitable versus nonrecruitable lung using CT imaging of
sure with the requisite that the chest wall elastance be near normal, the chest. A. The frequency distribution of the overall study group according to the percentage
and respiratory muscles are relaxed. of potentially recruitable lung (expressed as the percentage of total lung weight). The per-
• Large tidal volumes inducing overdistension of aerated lung regions centage of potentially recruitable lung was defined as the proportion of lung tissue in which
causes VILI. aeration was restored at airway pressures between 5 and 45 cm H O. B. CT slices obtained 2 cm
2
• Tidal hyperinflation could occur in a subset of ARDS patients even above the dome of the diaphragm at airway pressures of 5 (left) and 45 (right) cm H O from a
2
patient with a lower percentage of potentially recruitable lung. The percentage of potentially
with tidal volumes less than 6 mL/kg.
recruitable lung was 4%, and the proportion of consolidated lung tissue was 33% of the total
High airway pressures in and of themselves do not produce alveolar lung weight. C. CT slices obtained 2 cm above the dome of the diaphragm at airway pres-
disruption. Trumpet players repetitively generate large airway pressure, sures of 5 (left) and 45 (right) cm H O from a patient in the group with a higher percentage
2
up to 150 cm H O, without pulmonary sequelae. The critical factor of potentially recruitable lung. The percentage of potentially recruitable lung was 37%, and
30
2
causing injury is lung overdistention, and hence the term—volutrauma. the proportion of consolidated lung tissue was 27% of the total lung weight. (Modified with
Increased lung stretch is best assessed in the pressure domain by the permission from Gattinoni L, et al. Lung recruitment in patients with the acute respiratory
transpulmonary pressure (alveolar minus pleural pressure). Trumpet distress syndrome. N Engl J Med. April 27, 2006;354(17):1775-1786.)
players generate such high airway pressures by generating high pleural
pressures and alveolar pressures such that the transpulmonary pres- of lung distension, becoming less accurate in patients with stiff chest walls
sure is not elevated. In critically ill patients, undergoing volume control (eg, patients with ascites). Patients with hypoxic respiratory failure are
mechanical ventilation, peak inspiratory pressure (PIP) is often used at commonly ventilated with very high inspiratory pressures, which may
the bedside as a surrogate for the degree of lung inflation. However, PIP produce transpulmonary pressures >20 to 25 cm H O, values occurring
2
is dependent on the resistive pressure drop arising from flow across the at TLC, and hence lead to overdistention of lung units and lung injury.
11
endotracheal tube and conducting airways, and is also dependent on Direct evidence for volutrauma stems from several observations.
the compliance of the respiratory system. Consequently, increased PIP Open-chest animals whose lungs were ventilated with peak pressures
may not be indicative of overdistension; plateau pressure obtained after of 15 cm H O for 15 minutes had an 850% increase in their filtration
2
occlusion of the airway following inspiration reflects alveolar pressure, coefficient. In contrast, the filtration coefficients of closed-chest ani-
but does not directly reflect pleural pressure due to the pressure dissi- mals increased by 31% with a PIP of 30 cm H O, and by 450% with a
2
pated in distending the chest wall and thus is not an accurate surrogate PIP of 45 cm H O. Animals in which lung expansion was limited did
2
section04.indd 441 1/23/2015 2:19:27 PM