Page 633 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 633
452 PART 4: Pulmonary Disorders
causes, they are at an even higher increased risk for development of Despite recent advances in therapy, the mortality rates reported in clini-
ALI or ARDS. On average, ALI develops early in the course of the cal trials in the past decade have ranged from ∼25% to more than 50%. 3-9,22
hospitalization in at-risk patients. In two, large multicenter observa- The lowest mortality rates have been achieved with low-tidal-volume venti-
tional cohort studies, ALI developed on average by hospital day 2 and lation, which also limited end-inspiratory (plateau) pressure. 3,4,22 Although
the vast majority within 4 days. 35,36 Patients with a direct injury to the no recent studies have explicitly examined the cause of death in nonsurvi-
lung developed ALI on average 3 days earlier than patients with an vors, previously the majority of deaths were found to be due to multiorgan
indirect injury. 35 failure or sepsis, while progressive respiratory failure accounted for a small
■ RISK FACTORS FOR THE DEVELOPMENT OF ALI minority of deaths (eg, ∼15%). 65,66
ALI and ARDS impact the health and lives of survivors beyond the
AND ARDS AND PREDICTION MODELS ICU. Long-term physical, neuropsychiatric, and cognitive impairments
Why certain individuals with the same precipitating cause develop ALI in ALI survivors are common and are associated with reduced quality
and ARDS while others do not is unknown. Some of this differential risk of life (see Chap. 15). 27-31,67-70 In the aggregate, these deficits are extreme
can be attributed to other acquired risk factors, such as chronic alcohol- examples of the post-intensive care syndrome, and they represent an
ism. In addition, certain individuals may have an inherent predisposition important aspect of the impact of ARDS.
37
to developing ALI or ARDS while others may have inherent protections
against ALI or ARDS. These considerations are discussed below. PATHOLOGY AND PATHOPHYSIOLOGY
ALI and ARDS arise from diverse populations. Within these popula-
tions, specific clinical variables may affect both the risk of ARDS and It can be useful to distinguish between the early phases of lung injury and
ultimate outcomes if ARDS develops. 34-36,38,39 Clinical variables and subsequent events, as the early phases are characterized by exuberant infla-
38,71,72
outcomes associated with an increased risk of ARDS include chronic m mation and the later phases by repair and fibrotic mechanisms.
alcohol abuse ; lack of diabetes ; hypoproteinemia ; age and gender ; By light microscopy, the early appearance is of interstitial and alveo-
41
13
37
40
severity of injury and illness as measured by injury severity score (ISS) lar edema, capillary congestion, and intra-alveolar hemorrhage with
or Acute Physiology and Chronic Health Evaluation (APACHE) score ; minimal evidence of cellular injury (Fig. 52-3). By electron micros-
13
and possibly cigarette smoking. The mechanistic underpinnings of copy, changes of endothelial cell swelling, widening of intercellular
42
these associations are the subject of ongoing research. Furthermore, junctions, increased numbers of pinocytotic vesicles, and disruption and
processes of care, including transfusion of blood products 13,43 and initial denudation of the basement membrane are prominent. Inflammatory
ventilator settings (eg, tidal volumes greater than 6.5 mL/kg PBW), 44,45 cell infiltration of the lung interstitium may be seen (particularly in
have been associated with an increased risk of ALI development. These ARDS complicating sepsis or trauma) as well as neutrophil sequestra-
observations highlight the influence of the heterogeneity of a diverse tion in alveolar capillaries. During this early exudative phase of diffuse
source population and diverse processes that impact on the development alveolar damage (DAD), pulmonary edema and its clinical effects are
of ALI and ARDS. most pronounced (see Fig. 52-3). It is also a time when manipulations
Based on the identified predisposing conditions and risk modifiers to decrease the rate of edemagenesis are most likely to have an impact
for the development of ALI, a recent study validated a Lung Injury as discussed below.
Prediction Score (LIPS) to identify patients at high risk for the develop- Over the ensuing days, hyaline membrane formation in the alveolar
ment of ALI. The LIPS has the potential to be used clinically to identify spaces becomes prominent. Hyaline membranes contain condensed
36
at-risk patients and prevention strategies directed at the at-risk popula- fibrin and plasma proteins. Intra-alveolar activation of the coagulation
tion identified are warranted. system results in the formation of the fibrin, while plasma proteins are
Human studies aimed at investigating genetic or molecular mecha- deposited in the alveolar space as part of the inflammatory exudate that
nisms that predispose or protect individuals from developing ALI leaks across the alveolar-capillary membrane. Inflammatory cells become
and ARDS must take into account the effects of these population and more numerous within the lung interstitium. As the process of DAD
environmental differences. The initial investigations into genetic deter-
minants of ALI have been promising, including the first successful
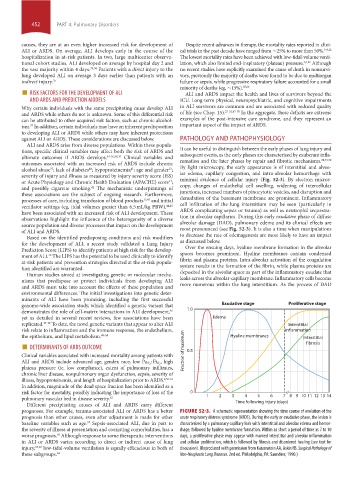
genome-wide association study, which identified a genetic variant that Exudative stage Proliferative stage
demonstrates the role of cell-matrix interactions in ALI development, 1.0
46
yet as detailed in several recent reviews, few associations have been Edema
replicated. 47-49 To date, the novel genetic variants that appear to alter ALI Interstitial
risk relate to inflammation and the immune response, the endothelium, inflammation
the epithelium, and lipid metabolism. 49-54 Hyaline membranes Interstitial
■ DETERMINANTS OF ARDS OUTCOME fibrosis
Clinical variables associated with increased mortality among patients with Fraction of maximum 0.5
, high
ALI and ARDS include advanced age, gender, race, low Pa O 2 : Fi O 2
plateau pressure (ie, low compliance), extent of pulmonary infiltrates,
chronic liver disease, nonpulmonary organ dysfunction, sepsis, severity of
illness, hypoproteinemia, and length of hospitalization prior to ARDS. 4,55-61
In addition, magnitude of the dead space fraction has been identified as a
risk factor for mortality, possibly indicating the importance of loss of the 0
pulmonary vascular bed in disease severity. 62 1 2 3 4 5 6 7 89 10 11 12 13 14
Different precipitating causes of ALI and ARDS carry different Time following injury (days)
prognoses. For example, trauma-associated ALI or ARDS has a better FIGURE 52-3. A schematic representation showing the time course of evolution of the
prognosis than other causes, even after adjustment is made for other acute respiratory distress syndrome (ARDS). During the early or exudative phase, the lesion is
baseline variables such as age. Sepsis-associated ALI, due in part to characterized by a pulmonary capillary leak with interstitial and alveolar edema and hemor-
57
the severity of illness at presentation and coexisting comorbidities, has a rhage, followed by hyaline membrane formation. Within as short a period of time as 7 to 10
worse prognosis. Although response to some therapeutic interventions days, a proliferative phase may appear with marked interstitial and alveolar inflammation
58
in ALI or ARDS varies according to direct or indirect cause of lung and cellular proliferation, which is followed by fibrosis and disordered healing (see text for
injury, 33,63 low-tidal-volume ventilation is equally efficacious in both of discussion). (Reproduced with permission from Katzenstein AA, Askin FB. Surgical Pathology of
these subgroups. 64 Non-Neoplastic Lung Diseases. 2nd ed. Philadelphia, PA: Saunders; 1990.)
section04.indd 452 1/23/2015 2:19:34 PM