Page 652 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 652
CHAPTER 53: Extracorporeal Lung Support 471
TABLE 53-1 Respiratory Conditions Requiring ECMO for Severe Hypoxemia TYPES OF EXTRACORPOREAL LUNG SUPPORT
Bacterial pneumonia ■ ECMO
Viral pneumonia
ECMO is a pump-driven, veno-venous, or veno-arterial circuit with an
Aspiration pneumonitis oxygenator to provide both oxygenation and ventilation.
Aspiration pneumonia
Acute respiratory distress syndrome ■ EXTRACORPOREAL CO REMOVAL
2
Pulmonary embolus Selective CO removal can be accomplished with low blood flow rates
2
(10 cc/kg/min) with the device attached with arteriovenous access (arte-
■ INCREMENTAL APPROACH TO THE MANAGEMENT rial cannula inserted into femoral artery, membrane oxygenator with
OF PATIENTS WITH SEVERE HYPOXEMIA venous cannula return to femoral vein, driving force is patient’s blood
pressure).
A potential complication is distal limb ischemia in the
27-31
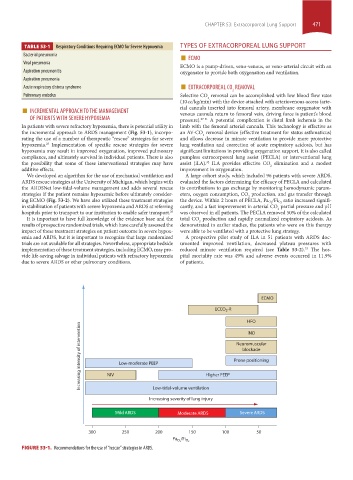
In patients with severe refractory hypoxemia, there is potential utility in limb with the femoral arterial cannula. This technology is effective as
the incremental approach to ARDS management (Fig. 53-1), incorpo- an AV-CO removal device (effective treatment for status asthmaticus)
2
rating the use of a number of therapeutic “rescue” strategies for severe and allows decrease in minute ventilation to provide more protective
hypoxemia. Implementation of specific rescue strategies for severe lung ventilation and correction of acute respiratory acidosis, but has
25
hypoxemia may result in improved oxygenation, improved pulmonary significant limitations in providing oxygenation support. It is also called
compliance, and ultimately survival in individual patients. There is also pumpless extracorporeal lung assist (PECLA) or interventional lung
the possibility that some of these interventional strategies may have assist (iLA). ILA provides effective CO elimination and a modest
32
2
additive effects. improvement in oxygenation.
We developed an algorithm for the use of mechanical ventilation and A large cohort study, which included 96 patients with severe ARDS,
ARDS rescue strategies at the University of Michigan, which begins with evaluated the factors determining the efficacy of PECLA and calculated
the ARDSNet low-tidal-volume management and adds several rescue its contributions to gas exchange by monitoring hemodynamic param-
strategies if the patient remains hypoxemic before ultimately consider- eters, oxygen consumption, CO production, and gas transfer through
2
ing ECMO (Fig. 53-2). We have also utilized these treatment strategies the device. Within 2 hours of PECLA, Pa O 2 /Fi O 2 ratio increased signifi-
in stabilization of patients with severe hypoxemia and ARDS at referring cantly, and a fast improvement in arterial CO partial pressure and pH
2
hospitals prior to transport to our institution to enable safer transport. 26 was observed in all patients. The PECLA removed 50% of the calculated
It is important to have full knowledge of the evidence base and the total CO production and rapidly normalized respiratory acidosis. As
2
results of prospective randomized trials, which have carefully assessed the demonstrated in earlier studies, the patients who were on this therapy
impact of these treatment strategies on patient outcome in severe hypox- were able to be ventilated with a protective lung strategy.
emia and ARDS, but it is important to recognize that large randomized A prospective pilot study of ILA in 51 patients with ARDS doc-
trials are not available for all strategies. Nevertheless, appropriate bedside umented improved ventilation, decreased plateau pressures with
implementation of these treatment strategies, including ECMO, may pro- reduced minute ventilation required (see Table 53-2). The hos-
33
vide life-saving salvage in individual patients with refractory hypoxemia pital mortality rate was 49% and adverse events occurred in 11.9%
due to severe ARDS or other pulmonary conditions. of patients.
ECMO
ECCO -R
2
HFO
Increasing intensity of intervention NIV Low-moderate PEEP Higher PEEP Prone positioning
iNO
Neuromuscular
blockade
Low-tidal-volume ventilation
Increasing severity of lung injury
Mild ARDS Moderate ARDS Severe ARDS
300 250 200 150 100 50
Pa /Fi
O 2 O 2
FIGURE 53-1. Recommendations for the use of “rescue” strategies in ARDS.
section04.indd 471 1/23/2015 2:19:50 PM