Page 71 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 71
40 PART 1: An Overview of the Approach to and Organization of Critical Care
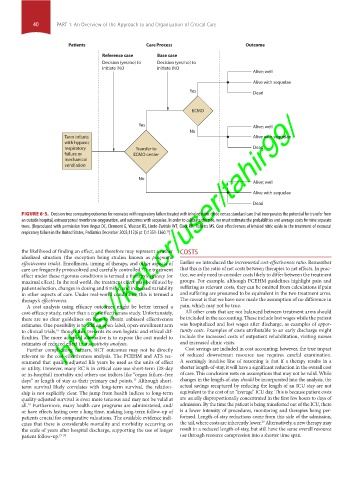
Patients Care Process Outcome
Reference case Base case
Decision (yes/no) to Decision (yes/no) to
initiate iNO initiate iNO
Alive; well
Alive with sequelae
Yes Dead
https://kat.cr/user/tahir99/
ECMO
Yes Alive; well
No
Term infants Alive with sequelae
with hypoxic
respiratory Transfer to Dead
failure or ECMO center
mechanical
ventilation
No
Alive; well
Alive with sequelae
Dead
FIGURE 6-3. Decision tree comparing outcomes for neonates with respiratory failure treated with inhaled nitric oxide versus standard care that incorporates the potential for transfer from
an outside hospital, extracorporeal membrane oxygenation, and outcomes with sequelae. In order to calibrate the tree, we must estimate the probabilities and average costs for nine separate
trees. (Reproduced with permission from Angus DC, Clermont G, Watson RS, Linde-Zwirble WT, Clark RH, Roberts MS. Cost-effectiveness of inhaled nitric oxide in the treatment of neonatal
15
respiratory failure in the United States, Pediatrics December 2003;112(6 pt 1):1351-1360. )
the likelihood of finding an effect, and therefore may represent a rather COSTS
idealized situation (the exception being studies known as pragmatic
effectiveness trials). Enrollment, timing of therapy, and other aspects of Earlier we introduced the incremental cost-effectiveness ratio. Remember
care are frequently protocolized and carefully controlled. The treatment that this is the ratio of net costs between therapies to net effects. In prac-
effect under these rigorous conditions is termed a therapy’s efficacy (or tice, we only need to consider costs likely to differ between the treatment
maximal effect). In the real world, the treatment effect may be diluted by groups. For example, although PCEHM guidelines highlight pain and
patient selection, changes in dosing and timing, and increased variability suffering as relevant costs, they can be omitted from calculations if pain
in other aspects of care. Under real-world conditions, this is termed a and suffering are presumed to be equivalent in the two treatment arms.
therapy’s effectiveness. The caveat is that we have now made the assumption of no difference in
A cost analysis using efficacy outcomes might be better termed a pain, which may not be true.
cost-efficacy study, rather than a cost-effectiveness study. Unfortunately, All other costs that are not balanced between treatment arms should
there are no clear guidelines on how to obtain unbiased effectiveness be included in the accounting. These include lost wages while the patient
estimates. One possibility is to add an open-label, open-enrollment arm was hospitalized and lost wages after discharge, as examples of oppor-
to clinical trials, though this presents its own logistic and ethical dif- tunity costs. Examples of costs attributable to an early discharge might
16
ficulties. The more accepted alternative is to expose the cost model to include the increased costs of outpatient rehabilitation, visiting nurses
estimates of reduced effect in a sensitivity analysis. and increased clinic visits.
Further complicating matters, RCT outcomes may not be directly Cost savings are included in cost accounting; however, the true impact
relevant to the cost-effectiveness analysis. The PCEHM and ATS rec- of reduced downstream resource use requires careful examination.
ommend that quality-adjusted life years be used as the units of effect A seemingly intuitive line of reasoning is that if a therapy results in a
or utility. However, many RCTs in critical care use short-term (28-day shorter length-of-stay, it will have a significant reduction in the overall cost
or in-hospital) mortality and others use indices like “organ failure–free of care. This conclusion rests on assumptions that may not be valid. While
days” or length of stay as their primary end points. Although short- changes in the length-of-stay should be incorporated into the analysis, the
17
term survival likely correlates with long-term survival, the relation- actual savings recaptured by reducing the length of an ICU stay are not
ship is not explicitly clear. The jump from health indices to long-term equivalent to the cost of an “average” ICU day. This is because patient costs
quality-adjusted survival is even more tenuous and may not be valid at are usually disproportionally concentrated in the first few hours to days of
all. Furthermore, many health care programs are administered, and/ admission. By the time the patient is being transferred out of the ICU, there
18
or have effects lasting over a long time, making long-term follow-up of is a lower intensity of procedures, monitoring and therapies being per-
patients crucial for comparative valuations. The available evidence indi- formed. Length-of-stay reductions come from this side of the admission,
29
cates that there is considerable mortality and morbidity occurring on the tail, where costs are inherently lower. Alternatively, a new therapy may
the scale of years after hospital discharge, supporting the use of longer result in a reduced length-of-stay, but still have the same overall resource
patient follow-up. 19-28 use through resource compression into a shorter time span.
Section01.indd 40 1/22/2015 9:36:54 AM