Page 70 - Hall et al (2015) Principles of Critical Care-McGraw-Hill
P. 70
CHAPTER 6: Assessing Cost-Effectiveness in the Intensive Care Unit 39
ProbabilityCost
Alive
Inhaled nitric oxide
Dead
https://kat.cr/user/tahir99/
Alive
Standard
Therapy
Dead
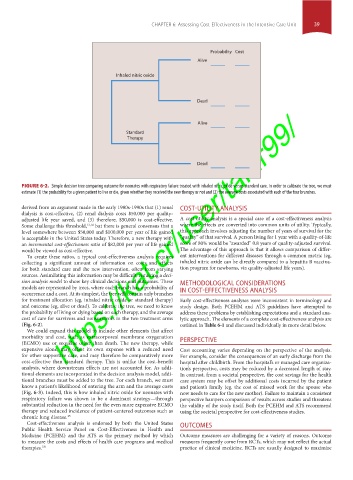
FIGURE 6-2. Simple decision tree comparing outcome for neonates with respiratory failure treated with inhaled nitric oxide versus standard care. In order to calibrate the tree, we must
estimate (1) the probability for a given patient to live or die, given whether they received the new therapy or not and (2) the average costs associated with each of the four branches.
derived from an argument made in the early 1980s-1990s that (1) renal COST-UTILITY ANALYSIS
dialysis is cost-effective, (2) renal dialysis costs $50,000 per quality-
adjusted life year saved, and (3) therefore, $50,000 is cost-effective. A cost-utility analysis is a special case of a cost-effectiveness analysis
Some challenge this threshold, 13,14 but there is general consensus that a where the effects are converted into common units of utility. Typically,
level somewhere between $50,000 and $100,000 per year of life gained this approach involves adjusting the number of years of survival for the
is acceptable in the United States today. Therefore, a new therapy with “quality” of that survival. A person living for 1 year with a quality-of-life
an incremental cost-effectiveness ratio of $82,000 per year of life gained score of 80% would be “awarded” 0.8 years of quality-adjusted survival.
would be viewed as cost-effective. The advantage of this approach is that it allows comparison of differ-
To create these ratios, a typical cost-effectiveness analysis requires ent interventions for different diseases through a common metric (eg,
collecting a significant amount of information on costs and effects inhaled nitric oxide can be directly compared to a hepatitis B vaccina-
for both standard care and the new intervention, often from varying tion program for newborns, via quality-adjusted life years).
sources. Assimilating this information may be difficult, requiring a deci-
sion analysis model to show key clinical decisions and outcomes. These METHODOLOGICAL CONSIDERATIONS
models are represented by trees, where each branch has a probability of IN COST-EFFECTIVENESS ANALYSIS
occurrence and a cost. At its simplest, the tree will contain only branches
for treatment allocation (eg, inhaled nitric oxide or standard therapy) Early cost-effectiveness analyses were inconsistent in terminology and
and outcome (eg, alive or dead). To calibrate the tree, we need to know study design. Both PCEHM and ATS guidelines have attempted to
the probability of living or dying based on each therapy, and the average address these problems by establishing expectations and a standard ana-
cost of care for survivors and nonsurvivors in the two treatment arms lytic approach. The elements of a complete cost-effectiveness analysis are
(Fig. 6-2). outlined in Table 6-1 and discussed individually in more detail below.
We could expand this model to include other elements that affect
morbidity and cost, such as extracorporeal membrane oxygenation
(ECMO) use or sequelae other than death. The new therapy, while PERSPECTIVE
expensive alone, may offset its own expense with a reduced need Cost accounting varies depending on the perspective of the analysis.
for other supportive care, and may therefore be comparatively more For example, consider the consequences of an early discharge from the
cost-effective than standard therapy. This is unlike the cost-benefit hospital after childbirth. From the hospital’s or managed care organiza-
analysis, where downstream effects are not accounted for. As addi- tion’s perspective, costs may be reduced by a decreased length of stay.
tional elements are incorporated in the decision analysis model, addi- In contrast, from a societal perspective, the cost savings for the health
tional branches must be added to the tree. For each branch, we must care system may be offset by additional costs incurred by the patient
know a patient’s likelihood of entering the arm and the average costs and patient’s family (eg, the cost of missed work for the spouse who
(Fig. 6-3). Indeed, this is how inhaled nitric oxide for neonates with now needs to care for the new mother). Failure to maintain a consistent
respiratory failure was shown to be a dominant strategy—through perspective hampers comparison of results across studies and threatens
substantial reduction in the need for the even more expensive ECMO the validity of the study itself. Both the PCEHM and ATS recommend
therapy and reduced incidence of patient-centered outcomes such as using the societal perspective for cost-effectiveness studies.
chronic lung disease. 15
Cost-effectiveness analysis is endorsed by both the United States OUTCOMES
Public Health Service Panel on Cost-Effectiveness in Health and
Medicine (PCEHM) and the ATS as the primary method by which Outcome measures are challenging for a variety of reasons. Outcome
to measure the costs and effects of health care programs and medical measures frequently come from RCTs, which may not reflect the actual
therapies. 7,8 practice of clinical medicine. RCTs are usually designed to maximize
Section01.indd 39 1/22/2015 9:36:53 AM