Page 100 - Cardiac Nursing
P. 100
9/0
M
P
0
pta
ra
e 7
g
009
96.
9-0
6 A
qxd
1 A
8:4
p06
9/2
K34
0-c
03_
LWB K34 0-c 03_ p06 9-0 96. qxd 0 9/0 9/2 009 0 0 8:4 1 A M P a a g e 7 6 A pta ra
LWB
LWBK340-c03_p069-096.qxd 09/09/2009 08:41 AM Page 76 Aptara
76 PA R T I / Anatomy and Physiology
effects. 81 The direct effects are secondary to occupation of the Neuropeptide Y
-adrenergic receptors and inhibition of norepinephrine release,
and the indirect effects occur through inhibition of the adrener- NPY is an amino acid peptide released with norepinephrine from
gic second messenger cAMP. 82,83 There are also M 1 , M 3 , and M 5 sympathetic nerve terminals. NPY has direct pressor effects and
receptors in the heart, which may have pharmacologic implica- also exerts a prejunctional modulation of the release of other neu-
tions. 84 Of clinical importance, the negative chronotropic and rotransmitters. For example, NPY inhibits the release of acetyl-
inotropic effects associated with the M 2 receptor are blocked by choline from vagal nerve endings, thus attenuating the effects of
atropine. the parasympathetic system on heart rate, atrioventricular con-
duction, and atrial contractility. 90,91 In addition, NPY potentiates
the postjunctional contractile effects of norepinephrine. In the
Co-transmitters mesentery, 30% of the sympathetic nervous system induced vaso-
At the preganglionic synapse, the primary neurotransmitter for constriction depends on NPY, 92,93 although the role of NPY
the sympathetic and parasympathetic nervous systems is acetyl- varies depending on the vascular bed. NPY is also associated with
choline. At the neuroeffector junction in the sympathetic nervous vascular remodeling (Y1 receptor) and angiogenesis (Y2). Phar-
system, the primary neurotransmitters are norepinephrine and its macologic strategies that promote angiogenesis but inhibit the
precursor, dopamine, whereas the primary neurotransmitter of pro-atherosclerotic effects of NPY may be useful in preventing or
94,95
the postganglionic fibers of the parasympathetic nervous system treating pathological vascular remodeling.
is acetylcholine. However, other neurotransmitters that augment
or modify the effects of the primary neurotransmitter are co- Vasoactive Intestinal Peptide
released, and are referred to as co-transmitters (Fig. 3-6). 85–87 The
most prominent co-transmitters in the sympathetic nervous sys- VIP is present in the peripheral and central circulation, where it
tem ganglia are NPY and ATP. 86,88 Vasoactive intestinal peptide acts as a nonadrenergic, noncholinergic neurotransmitter, or neu-
(VIP) is the prominent co-transmitter in the parasympathetic romodulator. Endogenous VIP is a potent vasodilator, although its
nervous system ganglia and nonadrenergic, noncholinergic effects vary in different vascular beds. It is released in response to
nerves. 89 vagal stimulation in the heart, where it produces coronary vasodi-
1. Transmitter release 2. Receptor 3. Receptor response
Presynaptic Receptors
ATP
Cotransmitters
NE A 1 α cellular signaling
NPY 2
ATP
α -adrenoceptor,
2
(α , α , α )
2B
2A
2C
NE Immediate effects
vasoconstriction
α -adrenoceptor,
1
(α , α , α ) vasodilatation
1A
1B
1D
, α , α )
(α 1H 1L 1N Trophic effects
β -adrenoceptor
1
(β , β , β )
3
2
1
Effector cell membrane
Adrenergic nerve terminal
Sympathetic cholinergic fiber
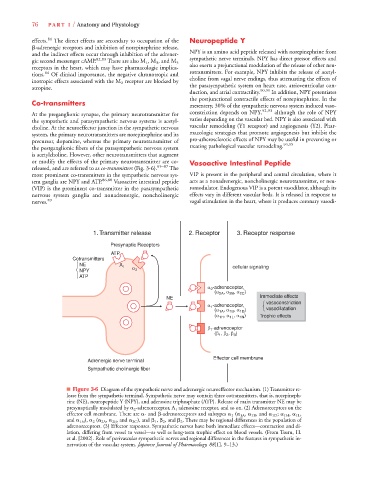
Figure 3-6 Diagram of the sympathetic nerve and adrenergic neuroeffector mechanism. (1) Transmitter re-
lease from the sympathetic terminal. Sympathetic nerve may contain three cotransmitters, that is, norepineph-
rine (NE), neuropeptide Y (NPY), and adenosine triphosphate (ATP). Release of main transmitter NE may be
presynaptically modulated by 2 -adrenoreceptor, A 1 adenosine receptor, and so on. (2) Adrenoreceptors on the
effector cell membrane. There are - and -adrenoreceptors and subtypes 1 ( 1A , 1B , and 1D ; 1H , 1L ,
and 1N ), 2 ( 2A , 2B , and 2C ), and 1 , 2 , and 3 . There may be regional differences in the population of
adrenoreceptors. (3) Effector responses. Sympathetic nerves have both immediate effects—contraction and di-
lation, differing from vessel to vessel—as well as long-term trophic effect on blood vessels. (From Tsuru, H.
et al. [2002]. Role of perivascular sympathetic nerves and regional differences in the features in sympathetic in-
nervation of the vascular system. Japanese Journal of Pharmacology, 88[1], 9–13.)