Page 101 - Cardiac Nursing
P. 101
9/2
009
9/0
9/2
009
8:4
8:4
0
0
96.
96.
9-0
9-0
qxd
0
9/0
qxd
0
e 7
7 A
g
e 7
7 A
ra
ra
pta
pta
M
M
1 A
1 A
P
a
g
P
a
LWB
K34
LWBK340-c03_p069-096.qxd 09/09/2009 08:41 AM Page 77 Aptara
L L LWB
K34
03_
03_
0-c
0-c
p06
p06
C HAPTER 3 / Regulation of Cardiac Output and Blood Pressure 77
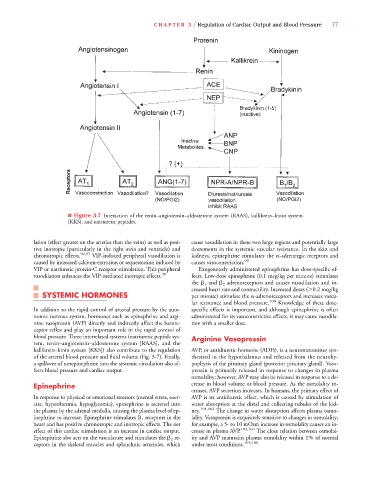
■ Figure 3-7 Interaction of the renin–angiotensin–aldosterone system (RAAS), kallikrein–kinin system
(KKS), and natriuretic peptides.
lation (effect greater on the arteries than the veins) as well as posi- cause vasodilation in these two large regions and potentially large
tive inotropic (particularly in the right atria and ventricle) and decrements in the systemic vascular resistance. In the skin and
chronotropic effects. 96,97 VIP-induced peripheral vasodilation is kidneys, epinephrine stimulates the -adrenergic receptors and
caused by increased calcium-extrusion or sequestration induced by causes vasoconstriction. 99
VIP or natriuretic protein-C receptor stimulation. This peripheral Exogenously administered epinephrine has dose-specific ef-
vasodilation enhances the VIP-mediated inotropic effects. 98 fects. Low-dose epinephrine (0.1 mcg/kg per minute) stimulates
the 1 and 2 adrenoreceptors and causes vasodilation and in-
creased heart rate and contractility. Increased doses ( 0.2 mcg/kg
SYSTEMIC HORMONES per minute) stimulate the -adrenoreceptors and increases vascu-
lar resistance and blood pressure. 100 Knowledge of these dose-
In addition to the rapid control of arterial pressure by the auto- specific effects is important, and although epinephrine is often
nomic nervous system, hormones such as epinephrine and argi- administered for its vasoconstrictive effects, it may cause vasodila-
nine vasopressin (AVP) directly and indirectly affect the barore- tion with a smaller dose.
ceptor reflex and play an important role in the rapid control of
blood pressure. Three interrelated systems (natriuretic peptide sys- Arginine Vasopressin
tem, renin–angiotensin–aldosterone system [RAAS], and the
kallikrein–kinin system [KKS]) also contribute to the regulation AVP, or antidiuretic hormone (ADH), is a neurotransmitter syn-
of the arterial blood pressure and fluid volume (Fig. 3-7). Finally, thesized in the hypothalamus and released from the neurohy-
a spillover of norepinephrine into the systemic circulation also af- pophysis of the pituitary gland (posterior pituitary gland). Vaso-
fects blood pressure and cardiac output. pressin is primarily released in response to changes in plasma
osmolality; however, AVP may also be released in response to a de-
Epinephrine crease in blood volume or blood pressure. As the osmolality in-
creases, AVP secretion increases. In humans, the primary effect of
In response to physical or emotional stressors (mental stress, exer- AVP is its antidiuretic effect, which is caused by stimulation of
cise, hyperthermia, hypoglycemia), epinephrine is secreted into water absorption at the distal and collecting tubules of the kid-
the plasma by the adrenal medulla, causing the plasma level of ep- ney. 101,102 The change in water absorption affects plasma osmo-
inephrine to increase. Epinephrine stimulates 1 receptors in the lality. Vasopressin is exquisitely sensitive to changes in osmolality;
heart and has positive chronotropic and inotropic effects. The net for example, a 5- to 10 mOsm increase in osmolality causes an in-
effect of this cardiac stimulation is an increase in cardiac output. crease in plasma AVP. 103,104 The close relation between osmolal-
Epinephrine also acts on the vasculature and stimulates the 2 re- ity and AVP maintains plasma osmolality within 1% of normal
ceptors in the skeletal muscles and splanchnic arterioles, which under most conditions. 105,106