Page 160 - Cardiac Nursing
P. 160
0
9/0
P
5 A
8:2
Apt
qxd
ara
36
e 1
52.
36
52.
P
M
9/2
009
p13
g
2-1
K34
0-c
06_
K34
LWB K34 0-c 06_ p13 2-1 52. qxd 0 9/0 9/2 009 0 0 8:2 5 A M P a a g e 1 36 Apt ara
L L LWB
LWBK340-c06_06_p132-152.qxd 09/09/2009 08:25 AM Page 136 Aptara
136 PA R T I I / Physiologic and Pathologic Responses
membrane and collagen fibers. Adherent platelets release The clotting factors are all present in the circulating blood in
adenosine diphosphate, which causes platelets to change from their inactive form until a stimulus for clot formation occurs.
their normal disc shape into a spherical form with pseudopods Twelve different substances have been officially designated as
that attach along the surface and allow platelets to clump to- clotting factors (see Table 6-2). As studied in the laboratory, the
5
gether. During activation, the platelets become sticky when coagulation process can be initiated by two different pathways:
bridges formed by fibrinogen in the presence of calcium cause the extrinsic pathway and the intrinsic pathway. Although differ-
platelets to adhere to each other, increasing the size of the entiating between them is helpful for understanding pathologic
platelet plug. Adenosine diphosphate and collagen also trigger mechanisms, medication actions, and coagulation tests, these two
formation of arachidonic acid from phospholipids in the pathways are functionally inseparable in vivo. The extrinsic path-
platelet membrane. Arachidonic acid leads to the formation of way, whose major mediators are rapidly inactivated, is the pri-
thromboxane A 2 , a substance that induces further platelet ag- mary initiator of the clotting cascade. The intrinsic pathway,
gregation. Thromboxane A 2 causes conformational changes in whose major mediators are more slowly degraded, is thought to
glycoprotein IIb/IIIa, a receptor on the platelet surface, which be important for maintenance and amplification of the clotting
exposes fibrinogen-binding sites. Fibrinogen builds bridges to cascade. Both extrinsic and intrinsic mechanisms eventually lead
adjacent platelets, a process called platelet adhesion, which ad- to the activation of factor X, with the remaining steps of the co-
vances platelet aggregation. When these aggregates are rein- agulation sequence being identical and referred to as the com-
5
forced with fibrin, they are referred to as a thrombus. Ulti- mon pathway. The sequence of the coagulation process is shown
mately, aggregated platelets plug the injured vessel. in Figure 6-2.
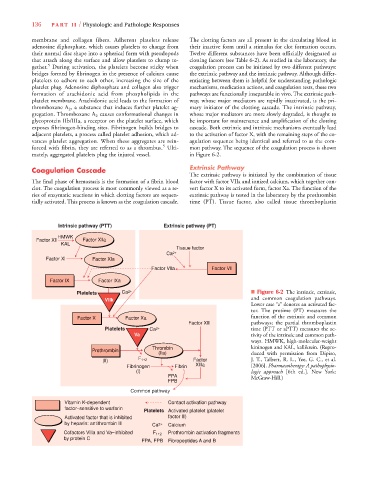
Coagulation Cascade Extrinsic Pathway
The extrinsic pathway is initiated by the combination of tissue
The final phase of hemostasis is the formation of a fibrin blood factor with factor VIIa and ionized calcium, which together con-
clot. The coagulation process is most commonly viewed as a se- vert factor X to its activated form, factor Xa. The function of the
ries of enzymatic reactions in which clotting factors are sequen- extrinsic pathway is tested in the laboratory by the prothrombin
tially activated. This process is known as the coagulation cascade. time (PT). Tissue factor, also called tissue thromboplastin
Intrinsic pathway (PTT) Extrinsic pathway (PT)
HMWK
Factor Xll Factor Xlla
KAL
Tissue factor
Ca 2+
Factor Xl Factor Xla
Factor Vlla Factor Vll
Factor lX Factor lXa
Platelets Ca 2+ ■ Figure 6-2 The intrinsic, extrinsic,
Vllk and common coagulation pathways.
Lower case “a” denotes an activated fac-
tor. The protime (PT) measures the
Factor X Factor Xa function of the extrinsic and common
Factor Xlll pathways; the partial thromboplastin
Platelets Ca 2+ time (PTT or aPTT) measures the ac-
Va tivity of the intrinsic and common path-
ways. HMWK, high-molecular-weight
Thrombin kininogen and KAL, kallikrein. (Repro-
Prothrombin
(lla) duced with permission from Dipiro,
(ll) F 1+2 Factor J. T., Talbert, R. L., Yee, G. C., et al.
Fibrinogen Fibrin Xllla [2006]. Pharmacotherapy: A pathophysio-
(l) logic approach [6th ed.]. New York:
FPA McGraw-Hill.)
FPB
Common pathway
Vitamin K-dependent Contact activation pathway
factor–sensitive to warfarin
Platelets Activated platelet (platelet
Activated factor that is inhibited factor lll)
by heparin: antithrombin lll Ca 2+ Calcium
Cofactors Vllla and Va–inhibited F 1+2 Prothrombin activation fragments
by protein C
FPA, FPB Fibropeptides A and B