Page 165 - Cardiac Nursing
P. 165
9/2
9/2
9/0
0
9/0
0
8:2
0
009
009
2-1
52.
2-1
p13
p13
qxd
0
qxd
52.
52.
8:2
41
41
e 1
g
e 1
ara
ara
Apt
41
Apt
M
P
M
5 A
5 A
a
g
a
P
P
K34
K34
L L LWB
K34
06_
06_
0-c
0-c
LWB
LWBK340-c06_06_p132-152.qxd 09/09/2009 08:25 AM Page 141 Aptara
C HAPTER 6 / Hematopoiesis, Coagulation, and Bleeding 141
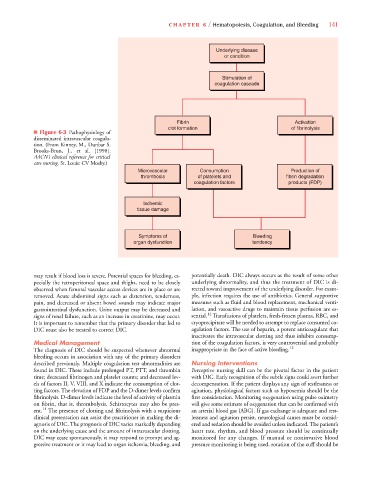
Underlying disease
or condition
Stimulation of
coagulation cascade
Fibrin Activation
clot formation of fibrinolysis
■ Figure 6-3 Pathophysiology of
disseminated intravascular coagula-
tion. (From Kinney, M., Dunbar S.
Brooks-Brun, J., et al. [1998].
AACN’s clinical reference for critical
care nursing. St. Louis: CV Mosby.)
Microvascular Consumption Production of
thrombosis of platelets and fibrin degradation
coagulation factors products (FDP)
Ischemic
tissue damage
Symptoms of Bleeding
organ dysfunction tendency
may result if blood loss is severe. Potential spaces for bleeding, es- potentially death. DIC always occurs as the result of some other
pecially the retroperitoneal space and thighs, need to be closely underlying abnormality, and thus the treatment of DIC is di-
observed when femoral vascular access devices are in place or are rected toward improvement of the underlying disorder. For exam-
removed. Acute abdominal signs such as distention, tenderness, ple, infection requires the use of antibiotics. General supportive
pain, and decreased or absent bowel sounds may indicate major measures such as fluid and blood replacement, mechanical venti-
gastrointestinal dysfunction. Urine output may be decreased and lation, and vasoactive drugs to maintain tissue perfusion are es-
12
signs of renal failure, such as an increase in creatinine, may occur. sential. Transfusions of platelets, fresh-frozen plasma, RBC, and
It is important to remember that the primary disorder that led to cryoprecipitate will be needed to attempt to replace consumed co-
DIC must also be treated to correct DIC. agulation factors. The use of heparin, a potent anticoagulant that
inactivates the intravascular clotting and thus inhibits consump-
Medical Management tion of the coagulation factors, is very controversial and probably
The diagnosis of DIC should be suspected whenever abnormal inappropriate in the face of active bleeding. 12
bleeding occurs in association with any of the primary disorders
described previously. Multiple coagulation test abnormalities are Nursing Interventions
found in DIC. These include prolonged PT, PTT, and thrombin Perceptive nursing skill can be the pivotal factor in the patient
time; decreased fibrinogen and platelet counts; and decreased lev- with DIC. Early recognition of the subtle signs could avert further
els of factors II, V, VIII, and X indicate the consumption of clot- decompensation. If the patient displays any sign of restlessness or
ting factors. The elevation of FDP and the D-dimer levels confirm agitation, physiological factors such as hypoxemia should be the
fibrinolysis. D-dimer levels indicate the level of activity of plasmin first consideration. Monitoring oxygenation using pulse oximetry
on fibrin, that is, thrombolysis. Schistocytes may also be pres- will give some estimate of oxygenation that can be confirmed with
ent. 11 The presence of clotting and fibrinolysis with a suspicious an arterial blood gas (ABG). If gas exchange is adequate and rest-
clinical presentation can assist the practitioner in making the di- lessness and agitation persist, neurological causes must be consid-
agnosis of DIC. The prognosis of DIC varies markedly depending ered and sedation should be avoided unless indicated. The patient’s
on the underlying cause and the amount of intravascular clotting. heart rate, rhythm, and blood pressure should be continually
DIC may cease spontaneously, it may respond to prompt and ag- monitored for any changes. If manual or noninvasive blood
gressive treatment or it may lead to organ ischemia, bleeding, and pressure monitoring is being used, rotation of the cuff should be